Sciatica
Unraveling What Causes Sciatica And Buttock Pain
Read More
October 11, 2023
If you are able to enjoy everyday actions such as standing, walking, or running, it is thanks to the sciatic nerves, which run from the lower back down the back of your legs. Understanding what causes sciatica and buttock pain is crucial, as you can think of these nerves as a “freeway” where signals relating to sensation and movement are transported from the lower part of your body to the brain and vice-versa.
When these nerves become trapped, irritated, inflamed, or damaged, they cause what’s known as “sciatica,” a painful condition that affects up to 40% of people at least once in their lifetime. Although sciatica is often a temporary condition that resolves itself with adequate care, it can sometimes derive from a more serious cause, such as tumor, bone overgrowth, and disc degeneration.
Because of this, it is essential to seek an accurate diagnosis and a sustainable line of treatment as soon as your symptoms appear. In this guide, we’ll look at how the Neurofunctional Pain Management approach pioneered by Relatyv can help you tackle systemic inflammation and chronic pain at the root of sciatica and pain in the buttocks without medications or surgery. Let’s dive in!
To better understand the symptoms, causes, and prognosis of sciatica, let’s start by looking at what sciatic nerves are and what happens when you develop sciatica.
Sciatic nerves are the longest and thickest nerves in the body, with a diameter of up to 3 quarters of an inch. These nerves emerge from the sacral portion of the spinal cord (L4 to S3 nerve roots) – your lower back. From here, the two sciatic nerves run through the buttocks and down the backs of the legs to reach the feet
Each sciatic nerve is, in fact, a bundle of nerves that split off just below the knee to connect the different components of the upper leg, lower leg, and foot to the central nervous system (the brain and spinal cord).
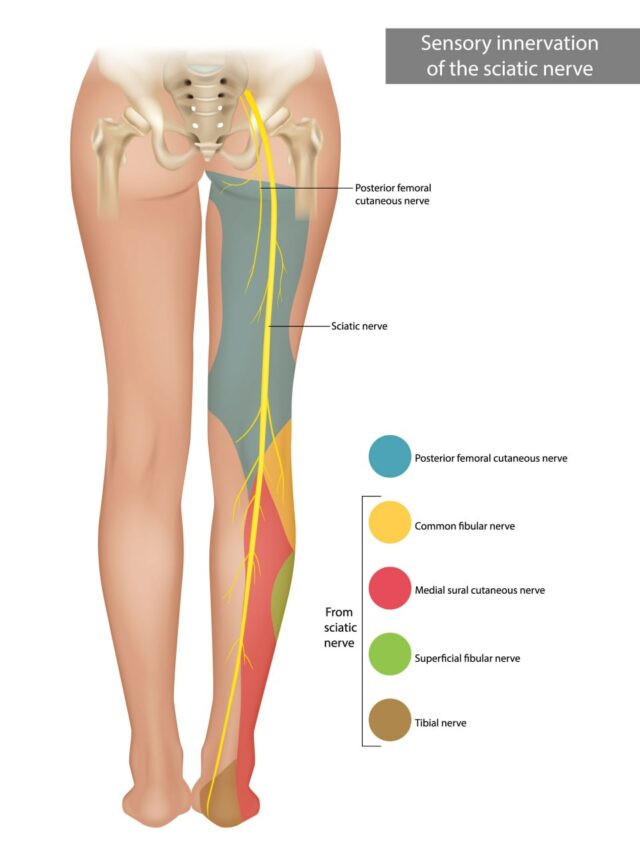
The main role of the sciatic nerve is to carry sensory and motor signals:
Sciatica refers to any medical condition or disorder that causes the sciatic nerves to become compressed, irritated, inflamed, or damaged. These conditions prevent the nerves from carrying signals to and from the brain as they are supposed to, which leads to nerve pain, numbness, and even temporary loss of movement.
Below, we’ll look at the symptoms, types, and causes of sciatica in more detail.
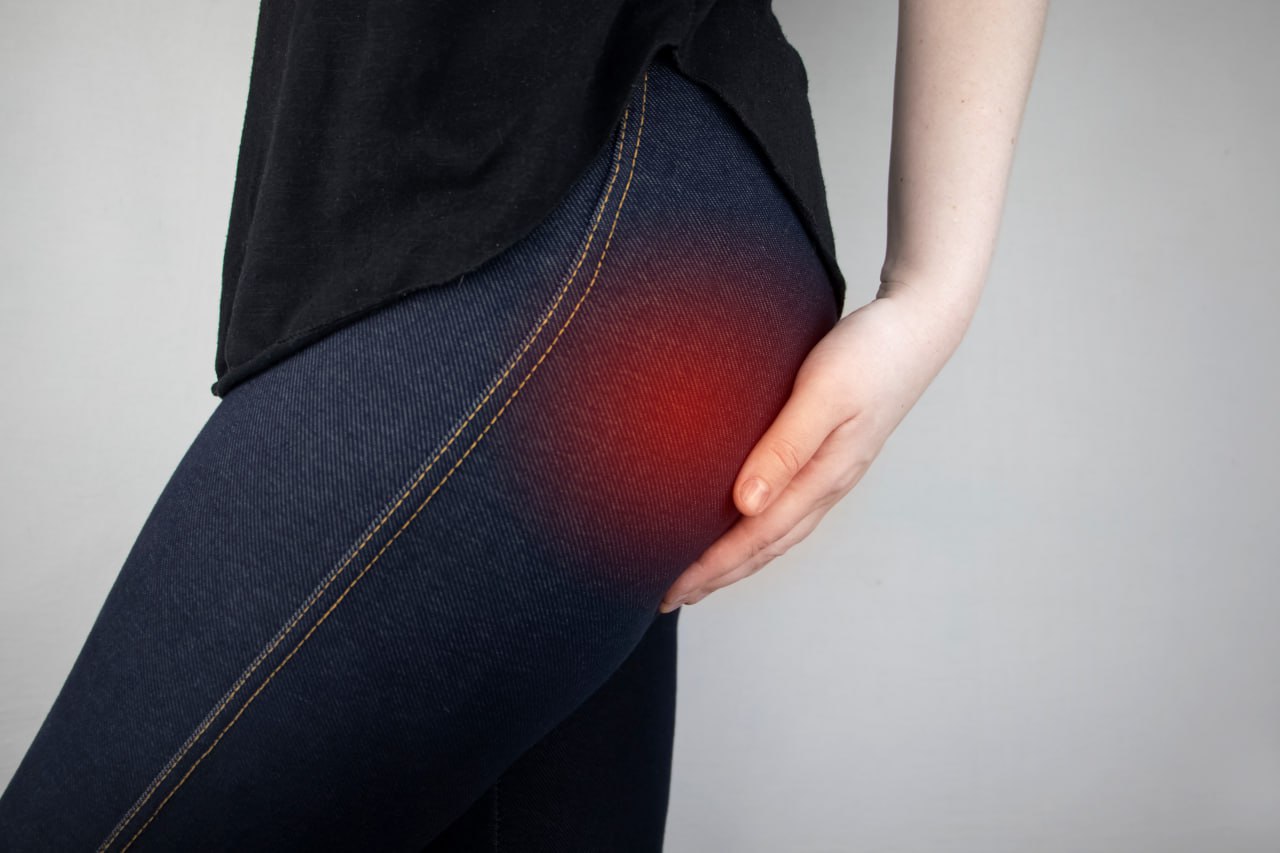
If you have been struggling with pain in the buttocks that is not going away, or you are experiencing numbness and loss of movement in the buttock area and upper leg, you may have sciatica or sciatica-like conditions.
Here’s the difference between the two:
Besides getting in the way of your everyday life, sciatica and pain in the buttocks can cause temporary disability and conceal more serious underlying conditions. To ensure you are getting adequate treatment in a timely manner, let’s look at what the symptoms and features of this condition are.
One of the most common symptoms of sciatica is pain, which tends to manifest with the following features:
As damage and irritation to the sciatic nerve worsen, you may begin to experience other symptoms, including numbness, tingling (“pins and needles” sensations, also known as paresthesia), weakness, and temporary loss of movement.
Commonly, sciatica begins to develop as pain in the buttocks. Over time, as irritation of the sciatic nerve progresses, symptoms such as pain, numbness, and tingling begin to spread along the length of the sciatic nerve.
In turn, you may begin to experience discomfort, weakness, and temporary loss of movement in your lower back, upper leg, lower, leg, or foot.
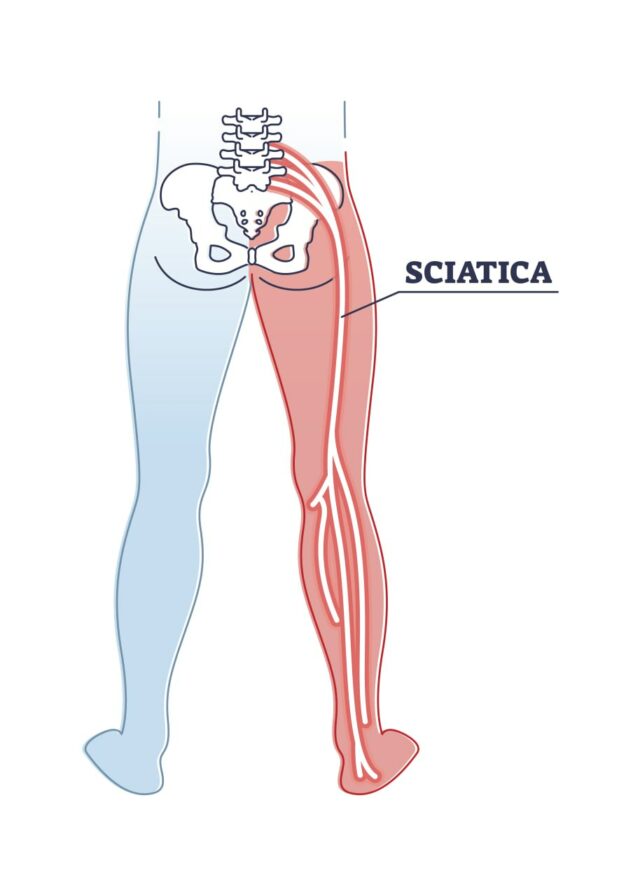
As we have seen above, the sciatic nerve is like a “freeway”: a bundle of several nerve fibers that carry signals to and from the brain. These signals relate to movement and sensations, such as pain and touch.
A pinched, irritated, or damaged sciatic nerve won’t be able to transmit signals as it is supposed to, resulting in symptoms such as extreme sensitivity to touch, nerve pain, numbness, and tingling.
In severe cases, damage to the sciatic nerve can interfere with the function of the nerves and muscles responsible for controlling the bladder and bowel. If you experience urinary or fecal incontinence, you should seek immediate medical care.
In most cases, sciatica is a temporary condition that improves within 12 weeks without serious complications. However, as we have seen above, pain in the buttocks can camouflage more serious, long-lasting conditions that require adequate treatment – including disc herniation, abnormal bony growths, and even tumors.
Because of this, it is crucial to learn more about the causes of sciatica and determine the best line of treatment to avoid life-limiting complications. Let’s look at the most common conditions at the root of pain in the buttocks below.
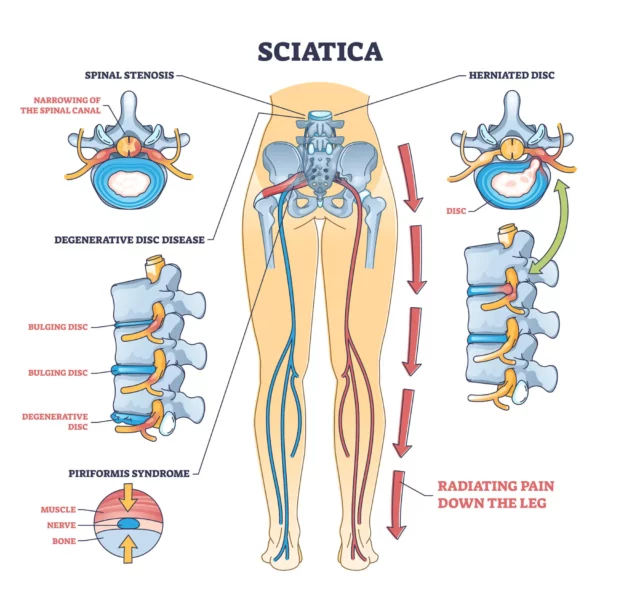
The spine is composed of small, circular bones, known as the vertebrae. These vertebrae are separated by the intervertebral discs, which are “cushions” of cartilage that allow movements such as flexion, extension, and rotation, and keep the spine flexible. They also protect the vertebrae from shock and friction damage.
Each intervertebral disc is composed of two main parts: an outer, stronger ring of cartilage and an inner, gel-like core. Although the intervertebral discs are incredibly reliable and capable of withstanding exceptional loads, factors such as overuse, aging, excessive stress, or injury can cause them to wear down.
When this happens, the outer ring of the intervertebral disc can become lax or crack, causing the softer core to protrude to nearby structures. Bulging or herniated discs can begin to press on, irritate, or damage adjacent spinal cord nerves, eventually leading to sciatica.
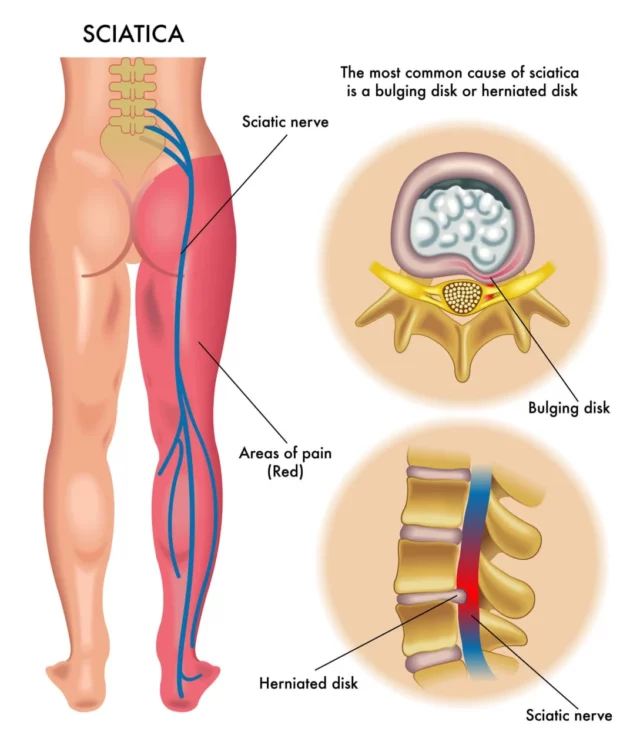
As the nerves are no longer able to transmit motor and sensory signals as expected, you may develop symptoms such as pain, numbness, and weakness.
Another common cause of sciatica is lumbar spinal stenosis. Spinal stenosis, or nerve compression, occurs due to the narrowing of the spinal canal, which is a cavity that houses the spinal cord. As this space in the spine narrows, the nerve roots are put under excessive pressure, which can interfere with the normal signaling of sensory and motor signals.
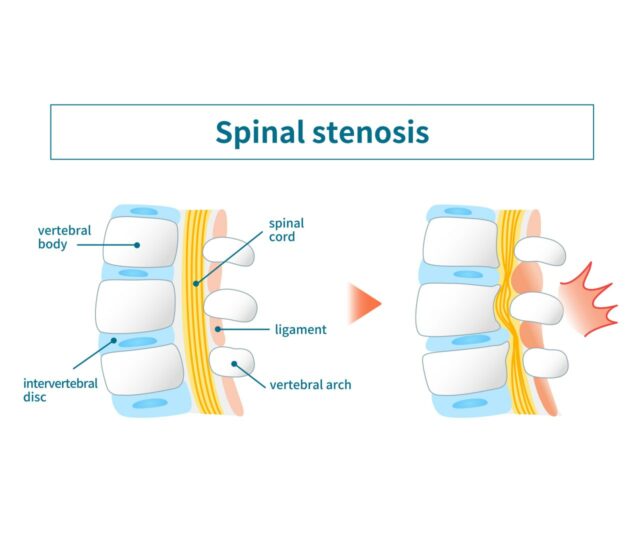
Spinal stenosis can occur due to several reasons and affect anyone, at any age. However, some common causes include:
Besides pain in the buttocks, lumbar spinal stenosis can cause a unique set of symptoms. Let’s look at these below.
Spinal stenosis causes ongoing nerve compression, which leads to severe pain that radiates from the area affected (the lower back, in this case) to the upper and lower leg. When the nerve roots in the spine are compressed or damaged, they can also misfire, causing several neuropathic pain (or nerve pain) conditions, such as:
Alongside misfiring and causing pain, compressed spinal nerve roots may also not be able to transfer sensory signals to the brain. This can lead to symptoms such as weakness and numbness, as well as a condition known as paresthesia.
Paresthesia refers to “pins and needles” sensations, which are often described as burning, prickling, itching, or “skin crawling” feelings. Depending on what nerve is affected by compression and irritation, these sensations can manifest in the hands, feet, buttocks, or other parts of the body.
Accounting for only 0.6 to 3% of lower back pain cases, piriformis syndrome (PS) isn’t as common as disc herniation or spinal stenosis. PS can feel like sciatica, but it requires a different line of treatment to address the root cause of your pain in the buttocks.
So, what is piriformis syndrome? PS is a neuromuscular condition that occurs when the piriformis muscle becomes inflamed, tingling, or swollen and compresses the sciatic nerve. The piriformis muscle is a narrow, flat muscle that runs from the lower spine, through the buttocks, to the top of the thigh.
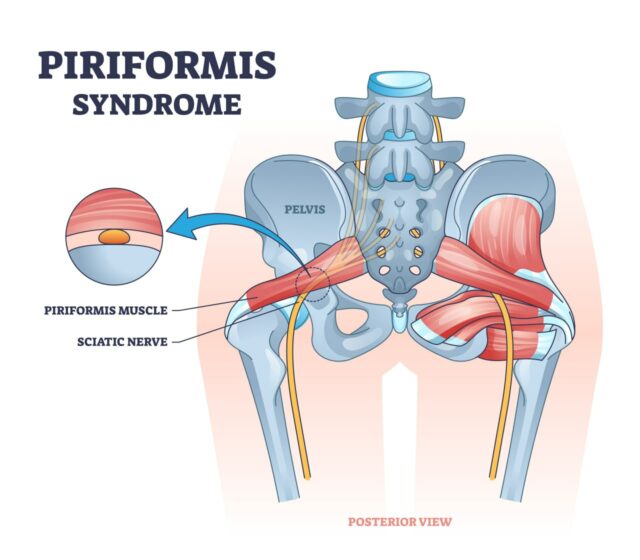
When this muscle becomes enlarged or tight, it presses on a specific area of the sciatic nerve, causing the pain and numbness to be localized to a certain site. The pain tends to become more intense during activities such as climbing stairs, walking, running, or sitting for long periods of time.
Some of the most common causes of PS include:
Degenerative disease is an incredibly widespread condition. It is estimated that up to 35% of adults over 30, and up to 90% of people aged 60, show signs of this disorder. However, not everyone will experience symptoms, and only 5% of low back pain cases can be traced back to degenerative disc disease.
This disease occurs due to the natural, age-related degeneration of the intervertebral discs, which are the discs located between the spine’s vertebrae. While it may affect anyone and its incidence increases with age, there are also some risk factors that may speed up the degeneration of the discs. These are:
Degenerative disc disease works similarly to herniated discs: as the intervertebral discs degenerate, the outer ring begins to protrude and crack, causing the inner gel-like substance to protrude and press on nearby spinal nerve roots.
The main difference between the two conditions is that degenerative disc disease is primarily caused by aging and wear and tear. Degenerative disc disease is also a common risk factor for herniated discs.
The sacroiliac joint is a joint located near the bottom of the spine, just above the tailbone, and connects the sacrum with the pelvis. It plays a vital role in stabilizing the spine during movements such as sitting or walking.
Dysfunction in the sacroiliac joint occurs when flawed or abnormal movements take place. These include:
Sacroiliac joint dysfunction does not cause sciatica but can cause sciatica-like pain in the buttocks, lower back, and hips, and can radiate down the leg (usually above the knee, but it can sometimes also affect the ankle and foot).
Besides pain, this condition can also cause numbness, weakness, tingling sensations, disturbed sleeping patterns, and difficulty in sitting.
In rare cases, sciatica and pain in the buttocks may be caused by tumors (abnormal growth of tissues) that press on and irritate the nerves within and around the spinal column. This can happen when the tumor is located near the spine or in the spinal canal. Some tumors that may appear as sciatic-like pain include:
Sciatica-like pain can also be caused by infections, such as blood vessel infections and spinal infections that develop into abscesses (swollen and infected masses).
Diabetes is considered to be the leading cause of peripheral neuropathy, or damage to nerves outside the brain and the spinal cord.
Today, up to 51% of people with diabetes are at risk of developing neuropathy. This is because the sharp rises and drops in blood sugar levels can eventually damage blood vessels. In turn, this can sever the supply of blood, oxygen, and nutrients to nerve endings, which, over time, degenerate and die.
Neuropathy can affect any nerve in the body and, although it is more common in the hands and feet, it can also affect the legs and buttocks, which causes symptoms similar to those of sciatica (especially in the legs).
Trauma or injury can lead to sciatica, pain in the buttocks, or conditions that mimic the symptoms of sciatica (e.g. lumbar spinal stenosis). This happens when fractures, ligament or tendon ruptures, and joint dislocations change the body’s mechanics.
Over time, improper mechanics can cause you to put more pressure on a certain aspect of the joint and prevent the body from distributing loads properly while walking, running, jumping, or lifting weights. When the areas affected are the spine, hips, buttocks, or legs, the sciatic nerve can become abnormally compressed or irritated during movement, thus leading to sciatica and sciatica-like pain.
Besides accounting for over 12% of the years of disability reported by people with chronic back pain, both obesity and being overweight have been seen to be major risk factors for sciatica and lumbar radicular pain.
There are several reasons for this:
Lastly, an unhealthy diet, excessive weight, and limited exercise can increase recovery time from sciatica and sciatica-like conditions.
Sciatica-like pain in the buttocks, as well as true sciatica, can derive from poor posture and abnormal body mechanics.
Poor sitting or standing posture (such as slouching or leaning forward to your desk) can increase strain in your lower back. At the same time, structural problems such as scoliosis can expose certain components that should be unaffected during movement to friction damage.
If not corrected promptly, poor posture and body mechanics can lead to undue pressure on nerves (such as the sciatic nerve) and associated symptoms, such as pain, numbness, and weakness.
Above, we’ve looked at some of the most common causes of sciatica and sciatica-like pain. However, there are also other risk factors that, over time, can significantly increase the likelihood of experiencing chronic pain in the buttocks.
Let’s look at these risk factors below.
Intervertebral disc degeneration is a normal aspect of the aging process. Over time, the discs lose their suppleness and flexibility, which increases the risk of herniation, tears, and bulging discs that can press on the sciatic nerve.
While you can’t turn back the hands of time, there is a lot that you can do to age healthily and control the rate at which intervertebral discs degenerate. For example, maintaining a healthy weight, eating healthily, and staying active are just some of the strategies to manage the complications of obesity, diabetes, and osteoarthritis – which are all risk factors for low back pain and pain in the buttocks.
Certain lifestyle factors increase your risk of developing sciatica or pain in the buttocks. These include:
Pregnancy and prolonged sitting can also put you at greater risk of developing sciatica or sciatica-like pain.
Both new and old injuries can impact your risk of developing sciatica.
New injuries may cause damage to the body components located around the sciatic nerve, such as the hip, leg, pelvis, or buttocks. Traumatic injury can compress or damage the sciatic nerve, thus leading to temporary symptoms
An old injury that hasn’t properly healed may have similar consequences. If a fracture, dislocation, or surgical intervention has permanently changed certain aspects of your body’s mechanics, you may be inadvertently putting unexpected pressure on your sciatic nerve during daily activities
If you have been struggling with sciatica or pain in the buttocks, the chances are that you’ve been recommended conventional lines of treatment, such as medications, physical therapy, or, in severe cases, surgery.
While these treatments may help you manage your pain and discomfort, they may not provide the long-lasting relief you are after. And, more importantly, they can expose you to undesirable side effects and risks.
Understanding the pros and cons of these treatment options is the first step toward finding a solution that works for your unique needs. Let’s start by looking at the common surgical and non-surgical lines of treatment commonly recommended for sciatic pain.
Non-surgical treatments are often the first port of call when you develop sciatica. After a few days of rest, you may resort to medications, physical therapy, and at-home remedies to manage the pain.
If you have been struggling with sciatica for months and other lines of treatments have not worked as well as you had hoped, your doctor may recommend surgery. It is important to be aware of the risks of surgical procedures before making this your treatment of choice: invasive procedures can increase the risk of infection and, while they may provide relief from sciatica, results may not be long-lived.
Here are two of the most common surgical treatments for sciatica:
Although sciatica and pain in the buttocks can affect anyone, at any age, there are preventive strategies you can take advantage of to reduce the risk of this condition becoming a chronic problem.
These measures can also help you recover quickly from an episode of sciatica and boost the effectiveness of the line of treatment you’ve chosen. Let’s look at preventive strategies in detail below.
Sitting is a normal aspect of our daily life. Whether you work at a desk, spend hours gaming or watching TV, or enjoy a sedentary hobby, you may inadvertently be spending a large part of your day sitting.
However, it is important not to underestimate the impact that sitting too much can have on your musculoskeletal and spinal health. Firstly, your entire upper body will rest on your lower back while sitting. This can increase the pressure on your buttocks and cause sciatica-like pain.
The poor posture you may adopt while sitting can also further compress your spine’s vertebrae, which can speed up disc degeneration and increase the risk of herniated or bulging discs. Lastly, prolonged sitting can weaken your back and core muscles, making injuries more likely.
Fortunately, you don’t need to revolutionize your entire lifestyle to cut down on sitting! Instead, try to introduce progressive changes, such as:
To prevent sciatica, another piece of the puzzle is physical activity and stretching. Boosting your muscle conditioning, endurance, and flexibility can help you avoid injuries and disorders such as piriformis syndrome.
Regular exercise is also key to keeping at bay several of the risk factors for sciatica, nerve pain, and pain in the buttocks, such as obesity, diabetes, osteoarthritis, and cardiovascular diseases.
Your back and core muscles work together to enable spinal movements, maintain stability during movement, and prevent injuries that may arise from overextension or excessive rotation. When your back muscles are weak, your body will rely on other, weaker structures to support these functions, such as ligaments and tendons. This can increase the risk of injuries and misalignments that can lead to chronic pain.
Strengthening your core muscles is an efficient way to support spinal movements, protect the spine, maintain a neutral pelvic tilt, and reduce stress on structures such as the vertebrae or intervertebral discs.
Excessive stress on your lower back can derive from multiple sources, including:
To decompress your lower back and find long-lasting relief from pain, work on losing excess weight, adopt a better posture, and work with an occupational therapist to prevent your job or hobby from compromising your spinal health.

When it comes down to overcoming pain in your bottom and finding a sustainable line of treatment that can help you regain your mobility and health, it is crucial to look at the root cause of your condition: inflammation.
Systemic inflammation can speed up the degeneration of the intervertebral disc and increase the risk of components of the spine becoming inflamed and swollen. Fortunately, tackling systemic inflammation – and deriving chronic pain – without surgery or medication is possible.
The Neurofunctional Pain Management approach pioneered by Relatyv addresses the root causes of- chronic pain and inflammation without resorting to taking drugs or fearing invasive procedures. This cutting-edge approach works by:
Let’s look at how this proprietary protocol works below.
Electroanalgesia involves high-pulse electrical stimulation that targets the intricate connections between pain, the nervous system, and the brain. This non-invasive therapy can intercept pain signals at the nerve’s source, providing relief at a cellular level. By regulating the responses of the nervous system, electroanalgesia has the potential to relieve the painful symptoms of osteoporosis-related microfractures.
At Relatyv, our protocols utilize specialized intravenous therapy (IV therapy) to support your bone health. This is an efficient approach that delivers important vitamins and minerals directly to the circulatory system, boosting their bioavailability and maximizing their impact. IV therapy aims to alleviate pain by reducing inflammation with immune support and to promote bone health by optimizing the body’s bone remodeling process.
At Relatyv, we are aware that painful experiences extend to more than just physical symptoms; they also affect your mental health and feelings of well-being. Our team of experts fosters an approach to pain management that encompasses the whole person. To assist people with osteoporosis in making informed lifestyle decisions, we provide individualized lifestyle counseling. We offer advice that includes addressing the strategies that promote bone health and may decrease the progression of osteoporosis, as well as creating a positive attitude about living with this long-term condition.
Our specialized protocols utilize a combination of these innovative Neurofunctional Pain Management techniques to collaboratively address the pain associated with osteoporosis without relying on invasive treatments or prescription medications. We believe it’s essential to find a pain management strategy that best suits you and your lifestyle.
Sciatica and pain in the buttocks can lead to temporary disability and rob you of several days’ worth of productivity and enjoyment. Fortunately, relying on medications while waiting for the symptoms to ease down or living in fear of having to undergo surgery are no longer the only options.
The non-invasive, non-chiropractic, and non-surgical approach pioneered by Relatyv – Neurofunctional Pain Management – can help you take back control of your musculoskeletal health and magnify your quality of life.
About the Author
Will is a healthcare executive, innovator, entrepreneur, inventor, and writer with a wide range of experience in the medical field. Will has multiple degrees in a wide range of subjects that give depth to his capability as an entrepreneur and capacity to operate as an innovative healthcare executive.
Share on Social Media


You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/
You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/
Neurofunctional Pain Management Overview
IV Therapy
Symptoms
Conditions Treated
Treatments
Articles by Category
Locations
Colorado
Wisconsin
Georgia
Hiram
Lawrenceville
Marietta
Powder Springs
Texas
Waco
Victoria
Illinois
Buffalo Grove
New Lenox
St. Charles
Arizona
Tucson
Waddell
Arlington
Avondale
Buckeye
Superior
Mesa
Palo Verde
Morristown
Tempe
Chandler
Anthem
Eloy
Florence
Fort McDowell
Phoenix
El Mirage
Coolidge
Gilbert
Arizona City
Casa Grande
Casa Blanca
Aguila
Sacaton
Apache Junction
Kearny
Stanfield
Goodyear
Litchfield Park
Alabama
Arkansas
California
Florida
Idaho
Michigan
Rhode Island
Minnesota
New Mexico
North Carolina
Ohio
Pennsylvania
South Dakota
Tennessee
Virginia

