Endometriosis

Addressing Endometriosis Pain With Intercourse
Read More
November 28, 2023
Endometriosis is a chronic inflammatory condition that affects over 6.5 million women in the US alone – but no two people will experience the same symptoms or impact on their lives. You may have nothing more than mild discomfort or, conversely, deal with debilitating pain, excessive bleeding, vomiting, fatigue, and infertility.
Over half of those with endometriosis also experience severe leg pain. Although this is often considered a secondary problem, it should not be overlooked: intense pain spreading through the buttock, leg, and foot can lead to mobility issues, reduced work performance, and disability, thus having a profound impact on your life.
But what can make it worse is the fact that, often, leg pain related to endometriosis is misdiagnosed and poorly managed, leaving sufferers to experience the worst consequences of their condition. Fortunately, there is a lot that can be done without resorting to medications or surgery.
The protocol pioneered by Relatyv – Neurofunctional Pain Management – uses a range of whole-person, non-invasive, and non-drug approaches to treat the systemic inflammation at the root of this symptom.
Beyond simply easing pain, Neurofunctional Pain Management can provide you with concrete tools to manage your condition and magnify your quality of life. Let’s explore what you need to know.
A lot is yet to be understood about how endometriosis causes leg pain. However, research has started to highlight the mechanisms that link these two conditions. To better understand what happens in your body when you experience endometriosis-related leg pain, let’s start by taking a step back and uncovering the dynamics of endometriosis.
The uterus, also called the womb, is the pear-shaped organ in a woman’s pelvis responsible for certain sexual and reproductive functions, including menstruation, gestation, and labor. The uterus is lined with endometrial tissue, also known as endometrium, which grows and thickens during the follicular phase of the menstrual cycle to prepare the womb for a fertilized egg.
During the early stages of pregnancy, the endometrium is responsible for providing the fertilized egg with the oxygen, nutrients, and protection needed to support fetal growth. However, if no egg is fertilized, the body sheds the endometrium through menstruation. During each menstrual cycle, new endometrium is formed and, if not needed, expelled through the vagina.
Endometriosis occurs when the endometrial tissue begins to grow outside of the uterus. These abnormal growths, known as endometrial implants, cause severe inflammation, cysts, scarring, and adhesions, which bind the organs in the pelvis together.
Left unaddressed, these complications can prevent organs from functioning normally and even lead to infertility, a complication reported by 30-50% of women with endometriosis. 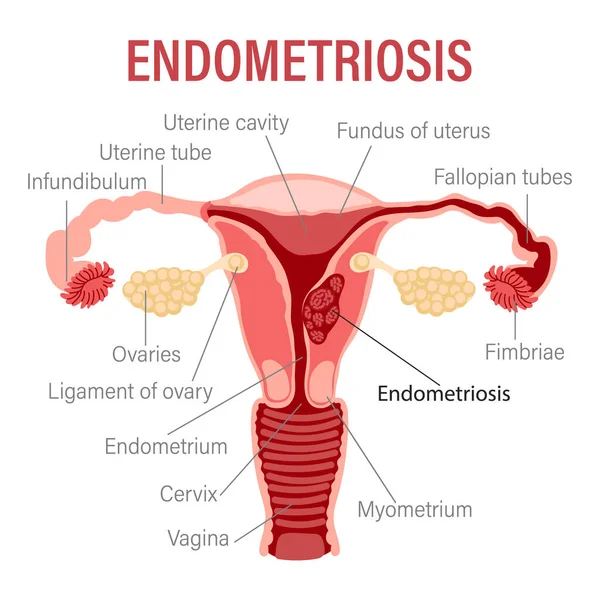
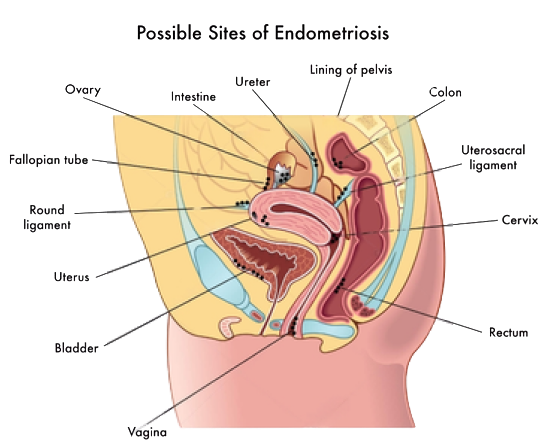
The endometrial implants can start to spread across organs and tissues surrounding the uterus, including:
What causes endometriosis to progress and worsen over time is the fact that the endometrial implants outside of the uterus behave in the same way as the endometrium inside the uterus.
Following the hormonal changes that occur during the menstrual cycle, the endometrial implants continue to grow and thicken during each cycle – but, unlike the endometrium inside the uterus, they can’t easily leave the body.
This process leads to the abnormal accumulation of endometrial tissue, which can cause trapped blood in the ovaries, blockages of the fallopian tubes, adhesions between organs, and scar tissue on reproductive organs.
The most common symptoms of endometriosis include severe pain during menstruation and intercourse, nausea and vomiting, excessive bleeding, pelvic pain, and pain when urinating or passing stools. However, in some cases, it can also cause leg pain.
This leg pain occurs when one or more of the nerves surrounding the uterus and other organs in the pelvis are inflamed, compressed, or damaged. When this happens, the transmission of motor and sensory signals to and from the brain is compromised.
This can lead to pain, numbness, and paresthesia (tingling and “pins and needles” sensations). These symptoms can be caused by several factors, including:
Leg pain is non-specific, which makes it difficult to diagnose properly. And it is even more challenging to determine with certainty whether this symptom arises from endometriosis.
Nonetheless, understanding what leg pain from endometriosis feels like is important, so you can seek adequate diagnosis and avoid taking medications for days on end – medications that do very little aside from masking symptoms and causing side effects.
Learning to identify when your symptoms are associated with endometriosis is even more crucial in light of the fact that around 90% of people experiencing the signs of this condition are disbelieved or dismissed by healthcare providers and loved ones alike.
Let’s start by understanding that leg pain from endometriosis is often described as stabbing or throbbing, and its intensity increases during menstruation (when the endometrial implants grow and thicken).
It can also feel different from the usual muscle cramping or soreness and can be associated with a pulling feeling in the leg, tingling sensations, numbness, or heaviness. The pain can be so severe as to prevent walking or physical activity and cause severe mobility issues for days each month.
Other symptoms include:
Here are the symptoms you may experience when your leg pain is caused by endometriosis.
When the nerves around the uterus are damaged or compressed, they become less efficient in sending and receiving signals relating to sensations and movement. These same nerves also spread toward and connect the lower extremities, which can lead to abnormal sensations in the legs.
Impaired sensory signals can lead to numbness, tingling, and “pins and needles” sensations, while damaged or compressed motor nerves will interfere with normal muscle movements. The combination of these two actions can result in feelings of heaviness in the legs, or a sensation that something is pulling or pushing the affected area.
If you have noticed that pain radiates from your pelvis to the lower back, through the leg, and toward the foot, you may have what’s known as sciatic endometriosis. This condition occurs when the endometrial implants grow on, compress, or cause lesions to the sciatic nerve.
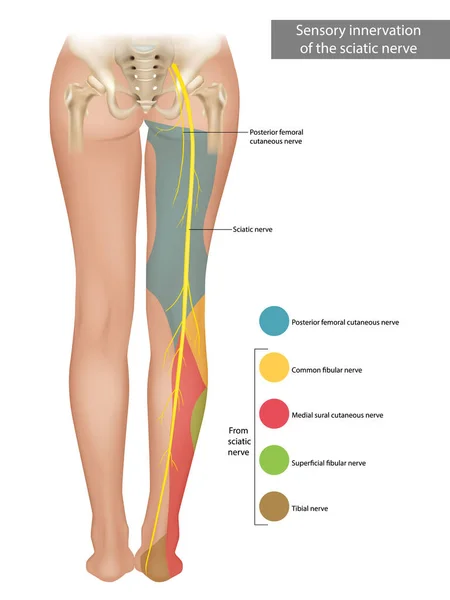
The sciatic nerve is the largest and longest nerve in the human body, running from the lower back down the back of each leg. It controls the muscles of the back of the leg and provides sensation to parts of the leg and the foot.
When this nerve becomes compressed or damaged, it can misfire, leading to sharp pain sensations that appear as sharp or stabbing. It can also lead to numbness, cramps, and spasms.
If the endometrial implants are affecting only the nerves on one side of the body, you are likely to experience pain in just one leg. This can be the case if the sciatic nerve is affected, or if the abnormal endometrial growths are affecting the obturator nerve, which controls the movement (adduction) of the thigh.
However, studies have shown that nearly 60% of women with endometriosis-related leg pain experience painful sensations and numbness in both legs.
This aspect is important in determining what’s causing your pain. For example, in people with leg pain caused by sciatica, the symptoms are commonly localized in one leg, as only one of the two sciatica nerves is usually affected. If both legs hurt at the time, the culprit may be endometrial growth.
You’ll know if your leg pain is stemming from endometriosis if the discomfort intensifies with menstruation. With each menstrual cycle, the endometrial implants continue to grow and thicken, adding up to inflammation and lesions.
During your menstruation, the body triggers a series of reactions to shed the unneeded endometrium, including cramping. These reactions can intensify the pain you experience, as well as the levels of inflammation caused by endometrial implants outside of the uterus.
Depending on what nerves are damaged or compressed by endometriosis, you may experience nerve pain in one or more locations in your lower extremities.
The nerves most commonly affected by endometriosis, due to their location, include:
Common areas of pain include:
Certain risk factors for leg pain related to endometriosis, such as height and age, are non-modifiable. However, other contributors, such as weight gain, stress levels, and lifestyle, can be modified through adequate interventions.
Additionally, some self-care strategies, home remedies, and medications may help relieve your symptoms. However, since these therapies won’t help in treating endometriosis and can lead to side effects, it is always recommended that you consult a specialized healthcare professional.
Let’s look at what you can do to address your symptoms below.
Heat packs, such as heating pads and hot water bottles, can provide relief from pain by relaxing muscles, easing tensions, and reducing cramping. Alternatively, ice packs applied to your legs or buttocks can slow down the blood flow around the affected area, thus reducing inflammation, swelling, and stiffness.
Consider trying out both strategies to find what works best for you. In either case, be sure to protect your skin from extreme heat or cold by wrapping the packs in a protective cloth.
According to a 2022 study, mindfulness meditation, breathing exercises, and mind-body activities like yoga may help relieve endometriosis pain. These activities provide beneficial effects by:
You may also consider working with a mental health professional to help you address the emotional and psychological effects of dealing with chronic pain.
Massage therapies, as well as alternative therapies such as acupuncture, may help relieve pain by easing muscle tension, stimulating the circulation of blood around the affected area, and inducing sensations of relaxation and well-being.
While massage therapy may help some patients with endometriosis, the outcomes can vary from one person to another and may not persist after a treatment is discontinued.
If self-care strategies and at-home remedies are not effective, certain oral medications can help. The most commonly prescribed therapies for endometriosis pain include:
Other options include vaginal valium, injections such as Botox, and anticonvulsants. Laparoscopic surgery to remove portions of the abnormal endometrial tissue may be recommended if other treatments have not worked or if the leg pain is interfering with your daily life.
Topical ointments, such as tiger balm, and pain-relieving creams, like topical ibuprofen, can help you manage leg soreness and pain, especially when it is localized to a certain area. Other commonly used topical medications include lidocaine, Icy Hot, and Voltaren.
When placed or rubbed on the painful and inflamed areas, topical treatments can temporarily reduce inflammation and pain. In the case of an irritated sciatic nerve, placing these medications on your lower back (which is where the sciatic nerve stems from), can provide an anti-inflammatory effect throughout the nerve and its branches.
With endometriosis, the pain you experience isn’t always related to the severity of your condition. You may have extensive endometrial implants and no pain – vice-versa, even mild endometrial growths can cause intense discomfort. Because of this, it is crucial to speak to a doctor immediately as soon as you notice any symptom that may relate to endometriosis.
In particular, you should seek medical care if:
It is important to keep in mind that if the endometrial implants have started to damage or irritate nerves, they can lead to permanent lesions and damage. This can cause you to develop severe or chronic neuropathy (nerve pain), which can persist even after treatments have removed the abnormal endometrial growths. Studies report that around half of people with endometriosis show signs of neuropathic pain and nerve damage.
Leg pain from endometriosis remains incredibly challenging to diagnose, especially when no other symptoms are present. However, if you suspect that you have endometriosis, your doctor may carry out a series of diagnostic tests to rule out other possible causes of leg pain, such as sciatica, peripheral artery disease, or deep vein thrombosis (DVT).
Some diagnostic tools your doctor may use include:
Certain tests for neuropathy, such as skin biopsies, nerve conduction tests, and electromyograms may also be used. These tests aim to determine the number of nerve fibers under the skin, as well as their capability to send and receive signals. Neurological tests may also be prescribed.
If you have endometriosis, you may be suffering from severe pain, discomfort, and disability for several days each month. And, over time, pain medications may become ineffective in helping you manage your symptoms, while also causing side effects.
However, a diagnosis of endometriosis does not have to be condemnation to living with severe pain or enduring inadequate treatments. Through Neurofunctional Pain Management, you can address the inflammation at the root of endometriosis-related leg pain and magnify your quality of life without medications or surgery.
About the Author
Will is a healthcare executive, innovator, entrepreneur, inventor, and writer with a wide range of experience in the medical field. Will has multiple degrees in a wide range of subjects that give depth to his capability as an entrepreneur and capacity to operate as an innovative healthcare executive.
Share on Social Media


You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/
You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/
Neurofunctional Pain Management Overview
IV Therapy
Symptoms
Conditions Treated
Treatments
Articles by Category
Locations
Colorado
Wisconsin
Georgia
Hiram
Lawrenceville
Marietta
Powder Springs
Texas
Waco
Victoria
Illinois
Buffalo Grove
New Lenox
St. Charles
Arizona
Tucson
Waddell
Arlington
Avondale
Buckeye
Superior
Mesa
Palo Verde
Morristown
Tempe
Chandler
Anthem
Eloy
Florence
Fort McDowell
Phoenix
El Mirage
Coolidge
Gilbert
Arizona City
Casa Grande
Casa Blanca
Aguila
Sacaton
Apache Junction
Kearny
Stanfield
Goodyear
Litchfield Park
Alabama
Arkansas
California
Florida
Idaho
Michigan
Rhode Island
Minnesota
New Mexico
North Carolina
Ohio
Pennsylvania
South Dakota
Tennessee
Virginia