Endometriosis is a lifelong, painful condition that affects 6.5 million women in the US alone, causes a loss of over six hours of productivity a week, and profoundly impacts a person’s professional and emotional life.
Nonetheless, surveys have shown that around 90% of people with endometriosis are disbelieved or dismissed by loved ones and healthcare professionals alike.
Thanks to advances in research, we now know that this condition and the symptoms that come with it are real and debilitating. But we also know that painkillers, hormonal therapies, and surgeries are no longer the only treatment options available to patients with endometriosis.
We’ll look at what endometriosis is and how Neurofunctional Pain Management programs may treat its symptoms without invasive procedures or medications. Let’s get started.
What Is Endometriosis?
To understand what endometriosis is and how it develops, it is firstly important to offer an overview of the female reproductive system.
In particular, the uterus – the pear-shaped organ in a woman’s pelvis, also called the womb – is the organ responsible for functions such as menstruation, gestation, and labor. The uterus is lined with endometrial tissue, which is called the endometrium.
The endometrium grows and thickens during the luteal phase of the menstrual cycle to prepare the uterus for a fertilized egg. If you become pregnant, the endometrium will support fetal growth by supplying oxygen and nutrients and will protect the embryo from microbial invasions during pregnancy.
However, if you are not pregnant, the body sheds the endometrium during your menstruation (period). New endometrium is created during each menstrual cycle.
Endometriosis develops when endometrial tissue begins to grow in areas outside of the uterus.
The abnormal growths of endometrial tissue – known as endometrial implants – may affect several organs and tissues around the uterus, including:
- Ovaries
- Fallopian tubes
- Ligaments around the uterus
- The pelvic cavity
- The exterior walls of the uterus
- Bladder
- Rectum
- Cervix
- Intestines
- Vagina
In severe cases, endometrial tissue can also be found in the diaphragm and chest.
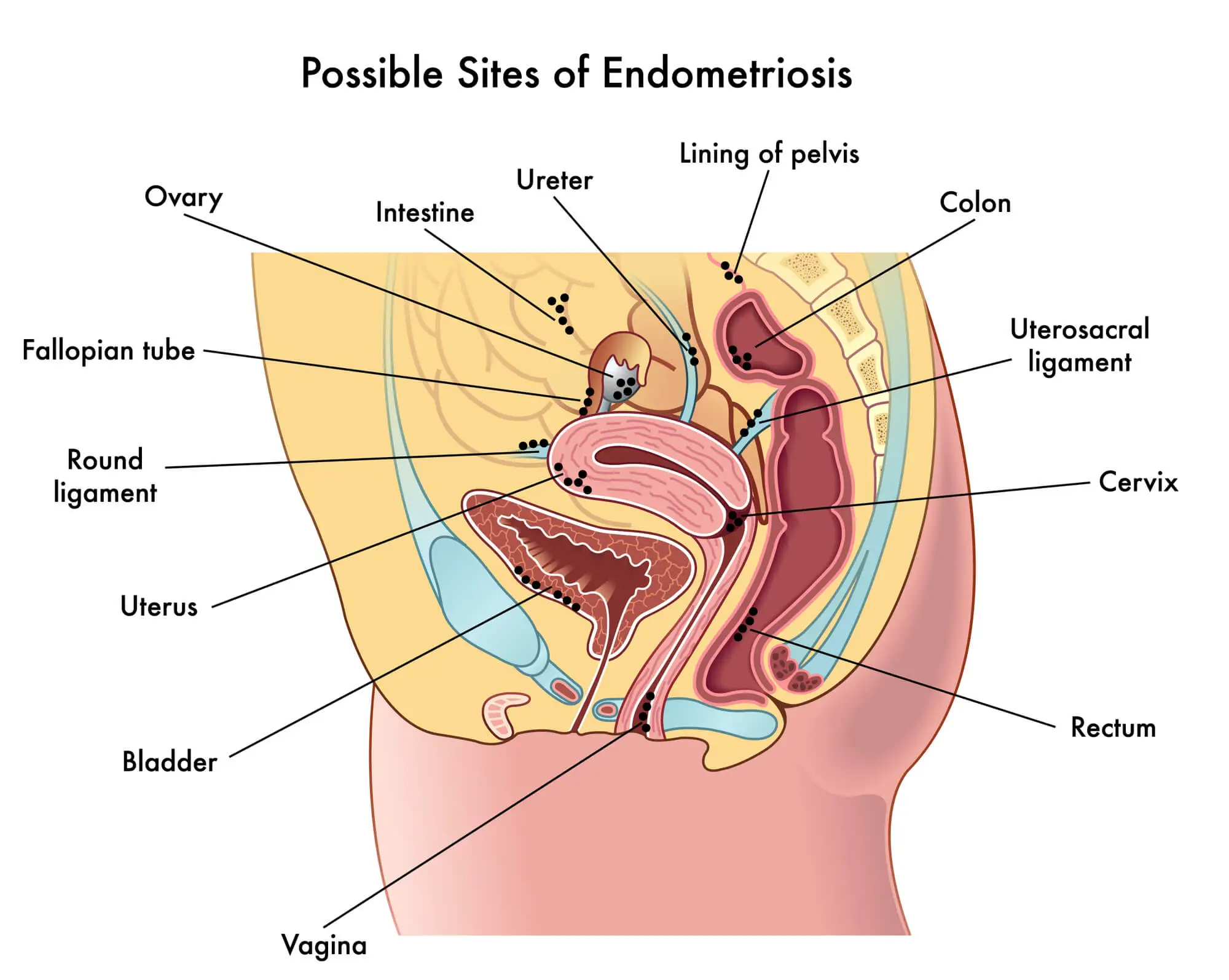
The build-up of abnormal endometrial tissue outside of the uterus can lead to a cascade of complications, including inflammation, scarring, and cysts. The tissue may also bind organs in the pelvis together, causing adhesions and preventing the organs from functioning as they should.
The endometrial tissue that grows outside of the uterus behaves in the same way as the tissue inside the uterus. This means that it responds to the hormonal changes that occur during the menstrual cycle and other events such as menopause.
So, during your cycle’s luteal phase, the endometrial implants will also grow, swell, and thicken. However, unlike the lining within the uterus, abnormal tissue that grows on other organs cannot easily leave your body during menstruation.
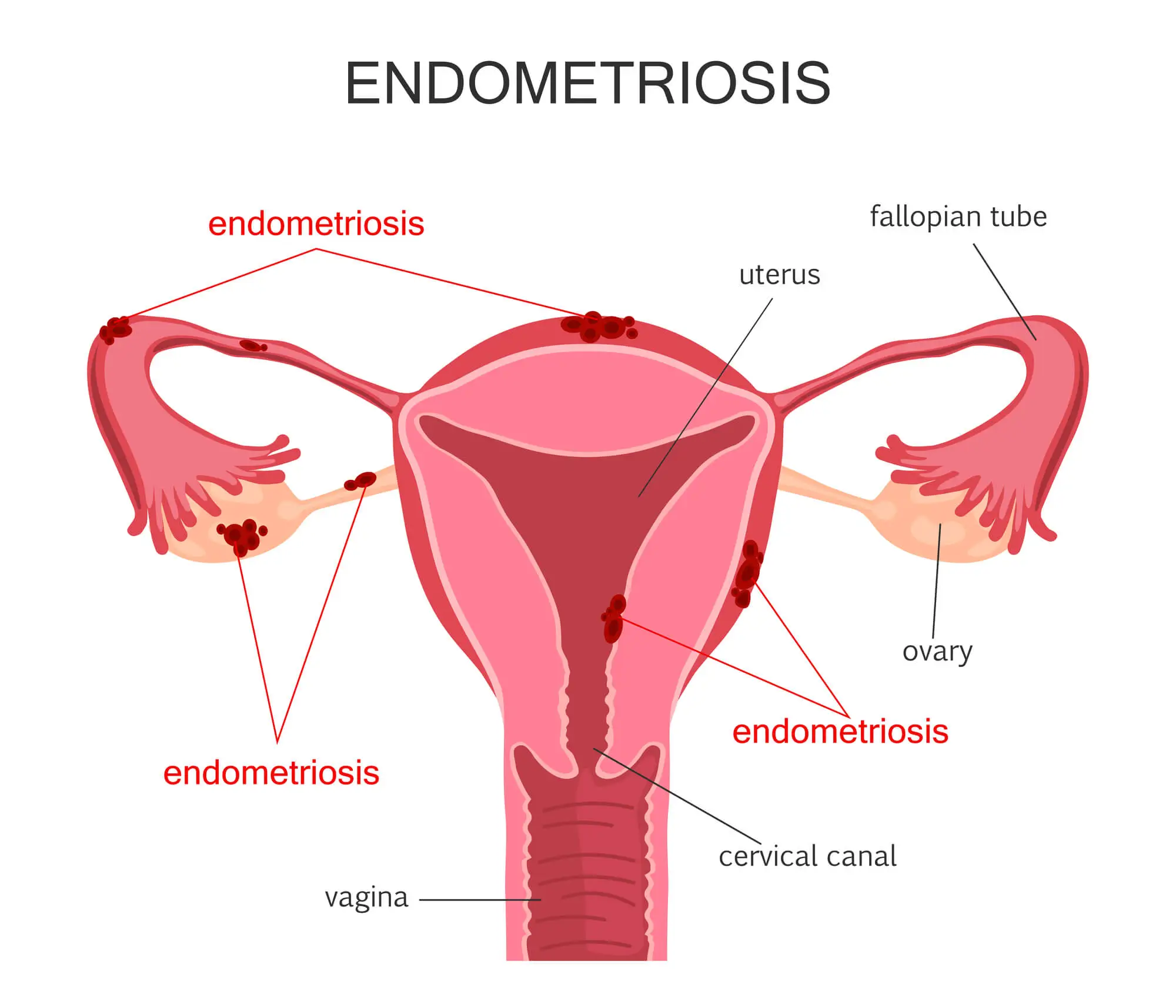
Over time, the accumulation of endometrial implants will expand and cause severe problems such as:
- Inflammation and swelling
- Blockages in the fallopian tubes
- Trapped blood in the ovaries, which may lead to cysts
- Adhesions between organs
- Scar tissue in the reproductive organs, which leads to infertility
- Problems with digestion and difficult bowel movements
The Stages Of Endometriosis Development
Endometriosis is generally classified into stages to describe the extent and location of the abnormal growth of endometrial tissue.
However, it is important to notice that the correlation between how far the endometrial tissue has spread and the severity of symptoms isn’t often straightforward. For example, some women may experience excruciating pain and severe symptoms even if they have a mild form of endometriosis or are in the early stages of the condition. Conversely, some patients have a severe form of endometriosis and only experience very mild discomfort.
Below, we’ll look at the stages of endometriosis in more detail.
- Stage 1: Minimal
Stage 1 endometriosis is characterized by minimal lesions and small wounds. During this stage, endometrial implants may affect your ovaries and cause inflammation in and around the pelvic cavity.
- Stage 2: Mild
As the abnormal endometrial growths continue to build up, you may experience stage 2 endometriosis. In this phase, the endometrial implants are still shallow and mostly affect the ovaries and pelvic lining.
- Stage 3: Moderate
Moderate endometriosis causes more and deeper implants, which are usually localized within the ovaries and pelvic linings but may extend to other organs. During this stage, you may also have small adhesions between organs, ovarian cysts, and lesions.
- Stage 4: Severe
Stage 4 endometriosis is the more severe form of this condition. It involves many deep implants that have spread through the ovaries, pelvic lining, fallopian tubes, and bowels. You may also have large cysts on one or both of your ovaries, as well as severe adhesions between organs.
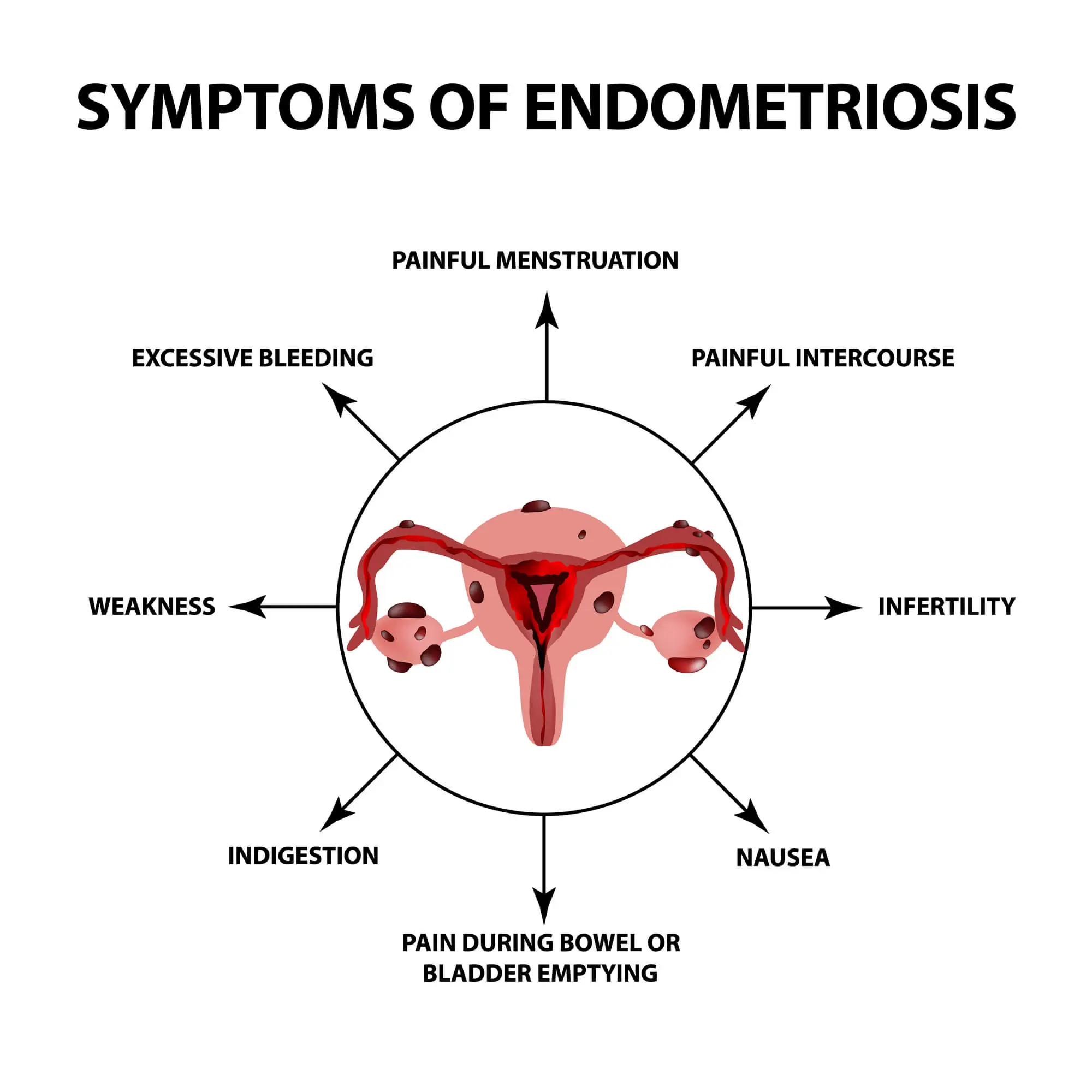
Symptoms Of Endometriosis
As we have seen above, the symptoms of endometriosis are not always correlated to the stage of the condition you are in. So, you may have stage 4 endometriosis and experience very little discomfort – and vice-versa.
Nonetheless, only around 20% of women with endometriosis are asymptomatic, and they often discover their condition when they deal with unexplained infertility. In the remaining 80% of cases, patients deal with chronic pain, painful periods, excessive bleeding, pain during intercourse, difficult bowel movements, digestive issues, and infertility.
These symptoms are often due to the endometrial implants outside of the uterus, which grow, thicken, and bleed during the menstrual cycle each month, but are unable to leave the body during menstruation. This leads to inflammation and irritation of the surrounding tissue.
Tissue scarring and thickening (fibrosis), as well as adhesions between organs, can contribute to discomfort and pain.
Below, we’ll look at the symptoms of endometriosis in more detail.
Painful Menstrual Periods
One of the most common symptoms of endometriosis is dysmenorrhea, or excessively painful menstrual periods, a condition that affects 70-93% of young women and causes missed days of work or school.
In the case of painful periods caused by a recognized pelvic condition such as endometriosis, this symptom is referred to as secondary dysmenorrhea.
Endometriosis causes painful periods because the endometrial implants respond to hormonal changes, and grow and bleed during the menstrual cycle. Dysmenorrhea manifests itself with several symptoms, including:
- Excessively painful menstrual cramps
- Back and abdominal pain during periods
- Back and abdominal pain between periods
- Cramps that begin 1-2 weeks before menstruation and extend 1-2 weeks after menstruation.
Pain With Sexual Intercourse
Another common symptom of endometriosis is pain during intercourse (dyspareunia), a condition that causes two-thirds of women with endometriosis to suffer from sexual dysfunction.
One of the reasons behind this symptom is that the inflammation of the endometrial growths is aggravated by the thrusting during penetration. However, in severe cases of endometriosis, the pain may also be due to the fact the endometrial implants bind the front wall of the rectum to the back wall of the vagina. These adhesions inhibit the mobility and expansion of the vagina during sex.
Some women with endometriosis only experience pain during deep penetration, or only have mild discomfort during sex. Others experience sharp and stabbing pain that may last for hours or days after sex.
The painful sensations may be more or less intense depending on the stage of your menstrual cycle.
Pain With Bowel Movements
Endometriosis can cause irregular and painful bowel movements. While the connection between these two conditions isn’t clear, the pain is often due to lesions and endometrial growth that occurs in the large bowel, bladder, rectum, or intestines.
The high levels of sustained inflammation, coupled with the thickening of the endometrial growth during the menstrual cycle, make passing stools painful. The painful sensations are often described as stabbing or sharp, and they are often accompanied by other gastrointestinal symptoms, such as constipation and bloating.
Excessive Bleeding
Endometriosis can change the frequency and nature of your menstruation. You may experience excessive bleeding or light bleeding (spotting) between periods.
Some changes in your periods that you may experience due to endometriosis include:
- Heavier periods with a consistently fast flow
- Shedding more blood each month
- Spotting or light bleeding between periods
- Scar tissue that may lead to internal bleeding
- Periods that last longer than seven days
- Bleeding after sex, often accompanied by pelvic pain
- Amenorrhea (absent periods)
- Bleeding through the rectum, usually after a bowel movements
The reason for these changes in the menstrual cycle is that people with endometriosis have more blood and endometrial tissue to shed each month.
Infertility
While a lot of the connection between endometriosis and infertility is yet to be understood, the correlation between these two conditions is undeniable.
According to a 2010 study published in the Journal of Assisted Reproduction and Genetics, 25-50% of infertile women have endometriosis, and 30-50% of women with endometriosis are infertile.
There may be several reasons why you have problems conceiving if you have endometriosis:
- Scar tissue caused by the endometrial implants in the ovaries may prevent the release of eggs cells
- The excessive growth of endometrial tissue can cause blockages in the fallopian tubes, thus preventing the egg cells from traveling to the uterus
- Endometrial implants can also damage a fertilized egg before it implants in the uterus, or inhibit the sperm.
- The sexual dysfunction and pain during sex many women with endometriosis experience may make it harder to conceive.
Women with endometriosis can still get pregnant and carry a baby to term successfully, sometimes with the help of fertility treatments such as in-vitro fertilization (IVF). Additionally, in the case of mild or moderate endometriosis, infertility may only be temporary.
Digestive Issues
Depending on where the endometrial growths are located, people with endometriosis may experience several gastrointestinal problems and digestive issues, a condition known as “endo-belly”.
This is due to several factors. Firstly, women with endometriosis are more prone to gastrointestinal bacterial overgrowth, which can cause changes in the digestive process. Additionally, the high levels of inflammations and the cysts caused by trapped blood in the ovaries may lead to bloating.
Endo-belly symptoms include the following:
- Constipation
- Diarrhea
- Bloating
- Nausea
A 2022 study has also shown that 10-52% of women with endometriosis also suffer from irritable bowel syndrome.
Another symptom of endometriosis is fatigue. Endometriosis-related fatigue becomes more evident during the menstrual cycle when the body attempts to eliminate abnormal or diseased tissue. During menstruation, the immune system attempts to combat endometriosis by releasing inflammatory toxins known as cytokines. These chemicals cause high levels of inflammation, which can lead to fatigue.
Muscle Spasm In The Stomach
Experiencing a muscle cramp can be painful and uncomfortable. While cramps can occur in any area of the body, muscle spasms in the stomach are particularly common. In fact, almost everybody will experience muscle spasms of some kind throughout their lifetime....
Painful Periods
Painful periods – a condition known as dysmenorrhea – are certainly not normal, and they can be a symptom of a more serious underlying condition. With an accurate diagnosis provided by our specialists and a tailored Neuragenex Neurofunctional Pain...
Endometriosis Pain With Intercourse
Dealing with pain during intercourse can be a source of significant distress and discomfort for both partners. In addition to the obvious physical pain, there is often an emotional toll that can be taken when dealing with sexual...
Stomach Pain
In most cases, stomach pain is nothing more than a temporary, minor issue that resolves itself in a matter of days. However, new surveys have found that 40% of the US adult population - or 60-70 million Americans - struggle with chronic disorders of the...
Painful Bowel Movements
The complex anatomy of the gastrointestinal tract and explore the negative implications that can come with experiencing painful bowel...
Digestive Issues
Digestive upset is a common issue we can all experience from time to time. However, if your digestive issues are an ongoing struggle and become more than just a minor inconvenience, perhaps they’re a sign of an underlying condition....
Infertility
The inability to conceive is a multifaceted issue that can be influenced by various factors and can also be a symptom of an underlying medical...
Stomach Is Swollen and Bloated
Abdominal bloating and swelling, also known as 'abdominal distention,' are two very common yet complex gastrointestinal complaints. Although these terms...
Causes Of Endometriosis
Endometriosis is considered to be an idiopathic disease. This means that the reasons why endometrial implants and scar tissue grow outside of the uterus are unknown.
However, since the discovery of endometriosis in the 1860s, several theories have attempted to look into the causes and risk factors of this condition. Currently, some of the most valid hypotheses include retrograde menstruation, the transformation of peritoneal and embryonic cells, and endometrial cell transport. Immune system disorders and surgical scar implantation may also be contributing factors.
Let’s look at these theories in more detail below.
Retrograde Menstruation
Retrograde or reverse menstruation may be one of the most likely causes of endometriosis. Retrograde menstruation is prevalent in 90% of menstruating women and occurs when endometrial tissue goes from the uterus back into the fallopian tubes and the abdomen instead of leaving the body during menstruation.
When the blood containing endometrial tissue flows back into the pelvic cavity, it may stick to the pelvic walls and organs, thus triggering endometriosis. These endometrial implants will then continue to spread and thicken with each menstrual cycle.
Induction Theory (Transformation Of Peritoneal Cells)
Another potential cause of endometriosis is described by what’s known as “induction theory”. According to this theory, unknown substances released by the endometrium in the uterus cause other cells in the body to transform into endometrial cells and grow outside of the uterus.
The most commonly affected cells in this process are the peritoneum mesenchymal stem cells, which are stem cells located in the inner side of the abdomen and stomach.
Embryonic Cell Transformation
Often, endometriosis begins during puberty. One of the theories that attempt to explain why this happens is the embryonic cell transformation hypothesis.
As a woman’s body prepares for menarche (the first menstrual cycle), the levels of estrogen in the body gradually increase. This usually happens during puberty.
The higher levels of estrogen may transform the embryonic cells in a woman’s body into endometrial-like cells that implant outside of the uterus. Embryonic cells are the cells responsible for the earliest stages of the human body’s development.
Surgical Scar Implantation
Endometriosis may also be caused by direct transplantation of the endometrial cells into organs and tissues (i.e.: the walls of the abdomen) that are located outside of the uterus.
This may happen during surgical procedures that involve the pelvic areas, such as a cesarean delivery (C-section) or hysterectomy (a surgical procedure used to remove parts of the uterus).
During these procedures, cells belonging to the endometrium in the uterus may contaminate organs or attach to the surgical incision.
Endometrial Cell Transport
In some cases, endometrial cells located within the uterus may be transported to other areas of the body via blood vessels or the lymphatic system. This happens similarly to how cancer cells are spread throughout the body.
Immune System Disorder
Studies conducted in 2022 attempt to define the role of the immune system in the development of endometriosis. Research has shown that certain disorders of the immune system may inhibit its ability to recognize, combat, and destroy endometrial cells that travel outside of the uterus.
Risk Factors For Endometriosis
Endometriosis may occur at any point during the reproductive age and affect any woman, but it is more likely to develop at some point after the first menstrual cycle (menarche).
Symptoms may develop over time and not become noticeable for several years. Often, in asymptomatic patients, a diagnosis of endometriosis is only achieved when investigating unexplained infertility.

While the idiopathic nature of endometriosis makes it hard to diagnose and treat, some risk factors may make you more prone to developing this disease during your lifetime. Let’s look at the risk factors in detail below.
Pregnancy History
If you have never given birth, you may be at greater risk of developing endometriosis.
This is because pregnancy temporarily stops the menstrual cycle and lowers the levels of estrogen in the body. In turn, this reduces the growth of endometrial cells inside and outside of the uterus.
If you already have endometriosis, pregnancy may temporarily reduce the intensity of your symptoms.
However, you can still develop endometriosis after carrying a baby to term. This is often due to the transfer of endometrial cells to organs outside of the uterus during a C-section.
Postpartum endometriosis may also occur in women who had long labor because the longer period of time between the rupture of the fetal membrane and delivery makes contamination and infections more likely.
Menstrual History
Some aspects of your menstrual history may make endometriosis more likely. These include:
- Starting your period at an early age, usually before 11
- Experiencing menopause at an older age
- Having menstrual cycles that are shorter than 27 days on average
- Having heavy periods that last longer than seven days
Having an early menarche and late menopause will increase your exposure to retrograde menstruation, while heavy or long periods may indicate an abundance of endometrial tissue. Both these factors may make endometriosis more likely.
Age
While the onset of endometriosis usually occurs during puberty, women in their 20s, 30s, and 40s are more likely to be diagnosed with this condition. This may also be because women in this age range may attempt to become pregnant and discover infertility problems.
Genetics
The prevalence of endometriosis in certain demographics may have a genetic factor, but no direct correlation has been established yet.
Generally, you may be at greater risk of developing this condition if one or more of your first-degree relatives (i.e.: mother, aunts, or sisters) have endometriosis. Having a family history of infertility may also be a genetic risk factor for endometriosis.
Higher Levels Of Estrogen
If your body produces excessively high levels of estrogen or you are exposed to this hormone throughout your lifetime, you may be at risk of endometriosis. This is because estrogen is responsible for supporting the growth and thickening of the endometrium during the menstrual cycle, which can make the build-up of endometrial tissue in and outside of the uterus more likely.
Low Body Mass Index
Endometriosis is more likely to occur in women with a slight, smaller frame, or low Body Mass Index (BMI). However, the connection between low BMI and endometriosis is unclear.
What’s more, in a new study, nearly 40% of the participants with endometriosis were overweight or obese, making a high BMI also a risk factor for endometriosis.
Medical Conditions That Block Menstrual Blood
Some medical conditions prevent the menstrual blood as expected, or flowing back into the fallopian tubes and ovaries, thus making endometriosis more likely.
Some of these medical conditions include abnormalities or obstructions in the uterus, vagina, or cervix.
Reproductive Tract Disorders
Some disorders of the reproductive tract can increase the risk of endometriosis.
- Uterine growths like polyps: Uterine growths may cause uterine bleeding, which can cause endometrial growths to be transported outside of the uterus. Uterine growths and polyps are both estrogen-dependent overgrowths, which means that the two conditions often coexist.
- Asynchronous uterine contractions: Uterine contractions are normal in a healthy uterus. When the pattern of these contractions becomes irregular, you may experience asynchronous uterine contractions. These can aggravate retrograde menstruation, thus making endometriosis more likely to develop.
How Endometriosis Is Diagnosed
Although endometriosis affects up to 11% of all women of reproductive age, most people experience a delay of nearly seven years in obtaining an accurate diagnosis.
However, over the past years, diagnostic protocols have improved to shorten this delay and ensure that women with endometriosis access adequate treatment as soon as possible.

Some of the tools used to determine a diagnosis of endometriosis include the following:
- Medical History: A healthcare provider – usually an Ob-Gyn – will assess your symptoms, review your medical history, and inquire about any previous pregnancies to determine whether you are at risk of endometriosis.
- Physical Exam: During a physical exam, a healthcare provider will palpate or manually feel your pelvis area to identify abnormalities such as cysts and scars, which may indicate the presence of endometrial tissue outside of the uterus.
- Ultrasound: Ultrasound tests use high-frequency sound waves to create images of the inner pelvic area. These tests can be used to determine the presence of endometrial implants outside of the uterus if these have not yet caused abnormalities that can be felt through physical examinations.
- Imaging Tests: Tests such as Magnetic Resonance Imaging (MRI) exams work similarly to ultrasound tests, but they use magnetic fields and radio waves to create detailed images of the organs in the pelvic area. These tests offer accurate insignia into the severity and location of endometrial implants.
- Laparoscopy: Laparoscopy is a minimally-invasive surgical procedure in which a surgeon will use a thin viewing instrument (laparoscope) to view the area inside the abdomen. This procedure can be used to determine the areas affected by endometriosis, collect tissue samples for testing, and remove parts of abnormal endometrial growth.
Treatment Options For Endometriosis
Sometimes, the symptoms of endometriosis may alleviate or disappear on their own, usually during health such as pregnancy or menopause. However, in most cases, the endometrial growths outside of the uterus will continue to grow with each menstrual cycle, causing the symptoms of this condition to aggravate over time.
If the symptoms become debilitating or life-limiting, a healthcare provider may recommend one or more lines of treatments to ease the pain and improve your quality of life.
However, given the consequences of some treatment options, women in their reproductive age must discuss their fertility goals before choosing a treatment plan for endometriosis.
Below, we’ll look at the treatment options that are most commonly recommended.
Hormonal Suppression
As seen above, endometrial implants – and endometriosis as a whole – are hormone-dependent. In turn, some hormonal therapies that aim to suppress certain hormones in the body may help slow down the progression of endometrial implants and ease the symptoms of this condition.
Some of the hormonal therapies often recommended for endometriosis include the following:
- Birth Control Pills: Birth control pills can include both estrogen and progesterone or be progesterone-only. These medications reduce the production of hormones that regulate the phases of the menstrual cycle, including ovulation and menstruation. In turn, birth control helps by reducing the flow and length of periods, while also slowing the growth of abnormal endometrial tissue.
- Gonadotropin-Releasing Hormone (GnRH) Medications: GnRH drugs work by stopping the production of the hormones that cause the menstrual cycle. When taking GnRH medications, you’ll experience a reversible and temporary “menopause”. This stops the production of endometrial tissue in and outside the uterus, which may help alleviate the symptoms of endometriosis.
- Pharmaceutical Hormone Suppressants: Drugs such as Danazol act by suppressing the hormones that cause you to menstruate. Taking these medications will stop you from having periods, and may temporarily prevent the endometrial growth from thickening and spreading.
When opting for these lines of treatment, you’ll have to take into account your plans of conceiving, as most hormone suppressants will stop you from getting pregnant. You should also note that the symptoms of endometriosis may come back as soon as you stop taking the medication, and the drugs seen above may come with significant side effects.
Over-The-Counter Pain Relief
Another option to manage the symptoms of endometriosis is over-the-counter pain medications and non-steroidal anti-inflammatory drugs (NSAIDs). While these medications may help you temporarily cope with the flare-ups of endometriosis, it is important to understand that they cannot be considered a sustainable long-term solution.
Indeed, taking NSAIDs over long periods can expose you to significant side effects, including stomach ulcers, increased risk of heart attack and stroke, and dependency. What’s more, painkillers may not work as efficiently for all patients with endometriosis.
Surgery
If you are dealing with life-limiting endometriosis pain, your doctor may suggest undergoing surgery. Surgical procedures are often seen as the last resort because they are invasive and come with significant complications and risks. What’s more, in 20% of cases, surgery is ineffective and patients require further treatment.
Two of the most common surgical interventions for endometriosis are laparoscopy and hysterectomy:
- Laparoscopy: Laparoscopy is a less invasive procedure used in milder endometriosis cases. During their procedure, a surgeon will perform small incisions in the lower abdomen, which are used to insert a long and thin viewing instrument. Once the surgeon has a clear understanding of the extent of the abnormal endometrial growth, he or she may decide to remove portions of it using thin instruments.
- Hysterectomy: This invasive surgical procedure is used to remove parts of the uterus, as well as the cervix and ovaries if needed. It is important to note that this procedure is irreversible and you’ll be permanently sterile.
Consequences Of Leaving Endometriosis Untreated
Although there is no permanent cure for endometriosis, it is important not to let this condition go unaddressed. Without adequate treatment, endometrial implants outside of the uterus will continue to grow with every menstrual cycle. This may lead to severe complications, such as the following:
- Infertility: Scar tissue and blockages in the fallopian tubes may prevent egg cells from leaving the ovaries and implanting in the uterus, which can lead to temporary or permanent infertility.
- Chronic Pain: When the fallopian tubes are clogged by endometrial growth, blood may become trapped in the ovaries. This leads to cysts, scar tissue, and adhesions, which can cause severe chronic pain. In turn, long-term pain can affect your mental health, cause you to miss days at work, and lead to depression, anxiety, and social withdrawal.
- Cancer: Abnormal endometrial growth can develop into a tumor, thus slightly increasing your risk of developing epithelial ovarian cancer. More research is needed to determine the correlation between these two conditions.
The Prevalence Of Endometriosis
The World Health Organization estimates that around 10% of women of reproductive age worldwide have endometriosis – a percentage that accounts for 190 million people globally. The condition is present in nearly 40% of infertile women and reaches peak prevalence in women aged 15 to 44.
While, at a glance, these statistics show how common endometriosis is, it is believed that the number of women with endometriosis is much higher. This is because this condition is often underdiagnosed or misdiagnosed.
What’s more, the prevalence of endometriosis may depend on race and ethnicity.
A 2019 study shows that, compared to White women, Black women are less likely to obtain an accurate diagnosis for endometriosis, while Asian women are more likely to receive a diagnosis. Research on the prevalence of this disease among other ethnic groups – including American Indian patients – is still limited. What’s more, on average, women wait between 8 and 12 years from the start of symptoms to be diagnosed with endometriosis.
Is There A More Effective Treatment?
As seen above, hormone suppressants are the first line of treatment for endometriosis. Although these may be efficient temporary solutions, they are not suitable for women looking to conceive. Additionally, birth control pills and other hormonal therapies come with severe side effects, such as mood swings, weight gain and loss, nausea, headaches, skin problems, and decreased sex drive.
On the other hand, surgical interventions may be even more problematic. According to a 2014 study, 62% of people who undergo a hysterectomy for endometriosis still have pain after the procedure and require further treatment. 31% of these required a second surgery. Among those who had both their uterus and ovaries removed, 10% still had pain and 4% required a second surgery.
So, is there a more efficient treatment option that does not come with such severe side effects? If you are battling endometriosis, the Neurofunctional Pain Management program may be the solution you’ve been looking for. Learn more about these lines of treatment below.
How Neurofunctional Pain Management Addresses Endometriosis Pain
When it comes down to finding a treatment for endometriosis that is both non-invasive and non-pharmaceutical, educating yourself about new approaches is critical. Among your options is Neurofunctional Pain Management®.
Neurofunctional Pain Management is a treatment program customized around the unique needs and goals of each patient. Each program leverages a combination of drug-free, non-surgical therapies and tools, such as electroanalgesia, nutritional hydration therapy, and lifestyle counseling to help patients magnify their lives.
Let’s look at this whole-person approach in more detail:
Electroanalgesia
Electroanalgesia is a pain management technique that uses high-pulse electrical current to ease pain, boost blood circulation, improve mobility, and induce...
IV Therapy
IV nutritional therapy, or intravenous therapy, involves administering vital nutrients directly to the bloodstream through an IV. This type of treatment bypasses the digestive system, allowing for maximum absorption and utilization of nutrients by the...
Lifestyle Counseling
Lifestyle counseling is an approach to managing chronic pain that involves identifying, assessing, and modifying lifestyle factors contributing to an individual's pain. For example, lifestyle factors such as nutrition, physical activity, stress, sleep quality...
Find A Solution For Endometriosis Pain
Endometriosis is certainly a chronic, life-limiting condition that can impact all aspects of your life, from your ability to be productive at work to your plans to conceive. However, dangerous surgical interventions and hormonal therapies are no longer the only options available to fight the pain you are experiencing.
With Neurofunctional Pain Management, you can regain control over your body and magnify your quality of life without medications or invasive procedures.
You can manage your endometriosis pain.