Plantar Fasciitis

Does Plantar Fasciitis Cause Swelling?
Read More
June 8, 2023
If you have plantar fasciitis, unbearable foot and heel pain accompanies even the simplest actions in your daily life, such as walking, climbing stairs, or enjoying your favorite sport or hobby.
The pain may be so intense that it can prevent you from moving your foot, being productive at work, or living independently. And, for many of the 2 million people suffering from this condition in the US alone, surgery represents the inevitable choice to ease their pain.
But taking medications daily, enduring the risks and side effects of surgery, or undergoing invasive procedures are no longer the only alternatives to regain the function and health of your foot.
Through the non-surgical, non-chiropractic, and non-pharmaceutical approach pioneered by Relatyv, you can regain your foot health and restore your quality of life without surgery or medications. Discover the whole-person Neurofunctional Pain Management approach below.
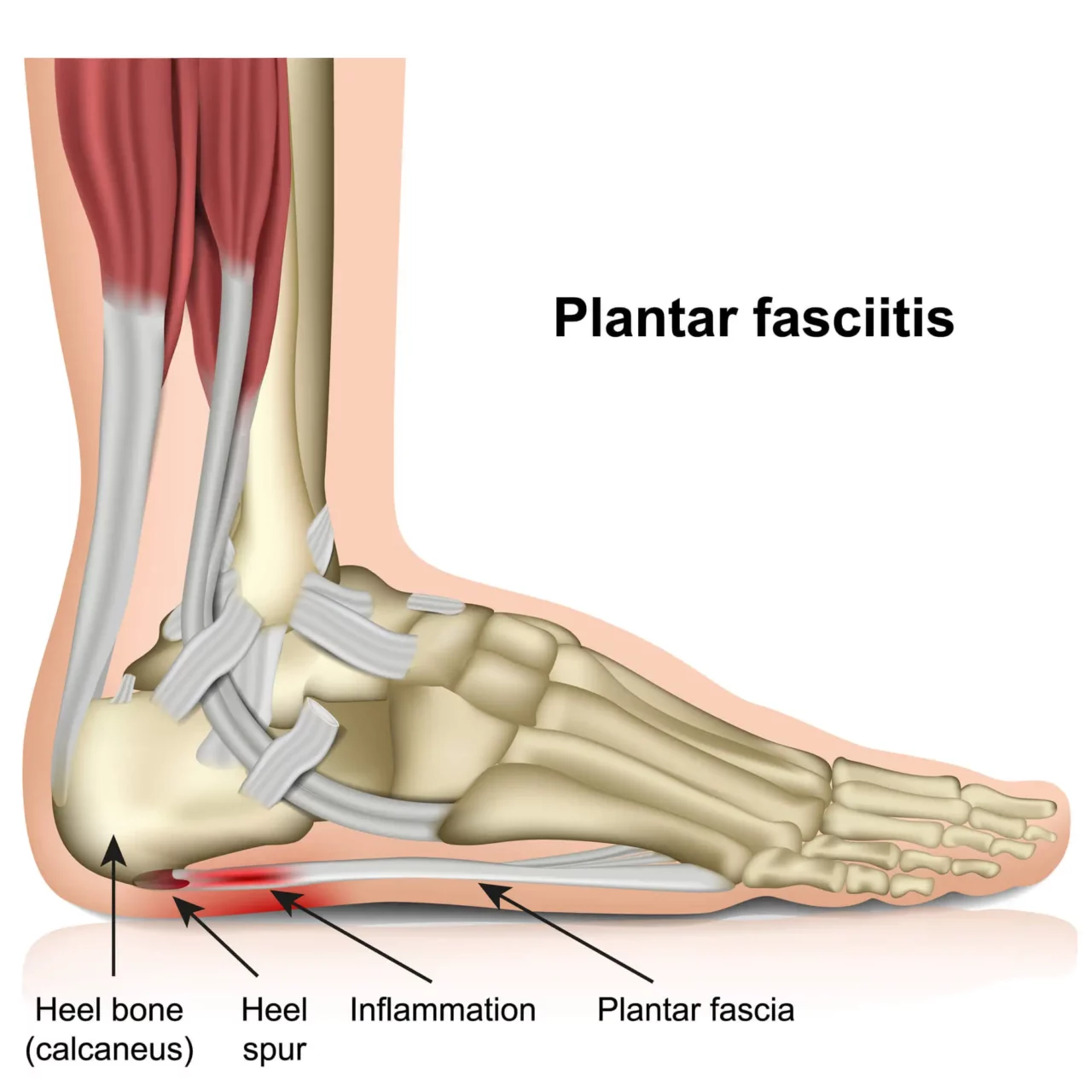
Plantar fasciitis is an inflammatory condition that occurs when the foot’s fascia becomes inflamed, irritated, or damaged. The fascia is a thick band of tissue that stems from the heel bone and then splits into smaller bands that fan out and attach to each toe. This component of the foot plays a vital role in stabilizing your gait, supporting the arch of the foot, and absorbing shock.
The fascia can become inflamed due to overuse, excessive or strenuous activities, inadequate footwear, and improper foot mechanics. An inflamed fascia leads to a cascade of symptoms, including pain, stiffness, swelling, and reduced range of foot motion.
Plantar fasciitis – a condition also known as plantar heel pain (PHP) – accounts for over half a million general and specialist care visits in the US alone, making it the leading cause of heel pain.
Although most patients report reduced pain and improved foot mobility with conservative therapies and medications, the pain may become so intense that it prevents you from being able to stand or walk. If all else fails, surgery may begin to appear as the inevitable choice.
The aim of plantar fasciitis surgery is to relieve tension in the fascia, ease inflammation, and reduce pain so that you can return to your daily activities and maintain proper foot mechanics. When your doctor suggests this line of treatment, it is important to understand the risks, benefits, and associated recovery times of this procedure. Let’s start by covering the basics.
Plantar fasciitis surgery is an approach to treatment that involves detaching the fascia from the heel bone.
After surgery, the fascia will heal by creating new connective tissue that stretches to and attaches to the heel bone, thus promoting the lengthening of the connective tissue. After the healing process is complete, a longer fascia can relieve tension, prevent further irritation, and increase foot mobility.
To achieve these results, your doctor may recommend one of two surgical interventions: fasciotomy or fasciectomy. Although they both have the same goal (to separate the fascia from the heel bone) they are performed in different ways:
Fasciotomy – also known as Plantar Fascia Release surgery – is the most common type of invasive intervention for plantar fasciitis, and can be either open or endoscopic.
Although endoscopic surgery is less invasive than open surgery, it involves a greater risk of damage to nearby tissues and nerves.
Other types of surgical interventions for plantar fasciitis exist, including gastrocnemius recession. This procedure is recommended if the inflammation of the fascia derives from short or thigh calf muscles (gastrocnemius muscles). It involves the surgical lengthening of these muscles to allow the ankle and foot to move more freely.
Given the side effects and risks that come with plantar fasciitis, surgery is often considered the last resort.
Usually, healthcare providers recommend various treatment options that aim to alleviate the pain from the fascia, improve mobility, and reduce inflammation. Some of the most common ones include:
These conservative treatments allow 80% of people with plantar fasciitis to make a full recovery from their condition within 12 months. However, 5% of people may require surgery.
This may be the case if:
If you suffer from chronic fascia pain, your condition may end up affecting your posture, gait, and foot mechanics, leading to severe complications and abnormalities in your legs, ankles, and spine. The pain can also prevent you from living a healthy and active lifestyle, thus exposing you to risks such as obesity, cardiovascular diseases, and diabetes.
In these cases, undergoing surgery may help you regain control over your life.
According to a 2017 study, plantar fascia release is successful in 70-90% of cases, in terms of reducing pain, improving patient mobility, and increasing activity levels. In particular, the results are excellent in over 88% of cases and good in over 6%, and pain relief maximizes at around 8 weeks after surgery. Full recovery is achieved between 6 and 18 months after surgery.
Additionally, around 75% of people who need surgery experience less pain than they did before surgical intervention. Nonetheless, it is important to note that surgery does not guarantee that your pain will go away entirely: around a quarter of patients continue to experience pain and discomfort after surgery.
Besides the fact that plantar fasciitis surgery isn’t always successful, this kind of procedure isn’t free of risks and side effects – including infection, nerve damage, and recurring pain. Understanding the possible complications of this line of treatment can help you make a more informed decision. Let’s get started.
One of the most common complications of plantar fasciotomy is surgical site infection. An infection may be caused by harmful bacteria that infiltrate the body during surgery.
While some infections are superficial and only affect the incision’s healing process, some can spread across the body and cause fever, chills, and drainage liquid. Surgical infections can increase your recovery time and need to be treated with antibiotics.
With 10-50% of patients left unsatisfied after fasciotomy, recurring heel or foot pain after surgery is a common complication that you should be aware of. This recurring pain may be due to different causes. For example, a nerve damaged during the procedure can lead to chronic pain.
Alternatively, the fascia release could fail to address the root cause of the irritation or inflammation, not offering the expected results.
Especially when undergoing endoscopic fascia release surgery, nearby nerves can become damaged or entrapped. This is commonly the case with Baxter’s nerve, which runs along the inside of the heel.
When a nerve connection is severed, nerve signals relating to movement, sensation, pain, and touch may be disrupted. This can cause symptoms such as spasms, numbness, tingling, and chronic or acute pain around the foot.
The incision necessary to release the fascia from the heel bone may inadvertently damage nearby components of the foot, including ligaments, muscles, and tendons. Although most of these injuries heal over time, they can slow down the recovery process and cause abnormalities in the foot’s mechanics.
The incision necessary to detach the fascia from the heel bone is minimal, which makes errors more likely. Over-releasing the plantar fascia – or detaching it too much from the heel bone – can cause the weakening and the flattening of the foot arch, which can lead to changes in the gait and deformity.
Some patients also experience the opposite complication if the fascia has not been released enough. This side effect requires follow-up surgeries.
The plantar fascia plays a vital role in stabilizing the foot’s mechanics during movement. Releasing the fascia from its attachment to the heel can impact these mechanics and create imbalances, leading to pain that could appear after surgery in other areas of the foot.
In particular, a 2002 study shows that surgical interventions that release over 50% of the fascia are likely to lead to lateral column pain, or pain affecting the bones that line the outer edge of your foot.
Surgery can help those with recalcitrant heel pain that has not improved with treatment options such as medication, rest, ice, and compression. However, given the severe side effects and lengthy recovery periods associated with fasciotomy, it is important to explore other conservative treatment options for plantar fasciitis such as the following:

Although these therapies may help you manage your pain during flare-ups, they are not an effective alternative to win over your chronic condition and regain your foot mobility. Here’s where Neurofunctional Pain Management comes in. Let’s discover the Relatyv approach below.
Pioneered by Relatyv, Neurofunctional Pain Management is a revolutionary whole-person approach that aims to help patients combat their pain condition without surgery or medications.
Neurofunctional Pain Management addresses all of those lifestyle factors that may be contributing to your pain and utilizes regenerative medicine therapies to support the body’s ability to fight inflammation and heal damaged tissue. In the treatment of chronic plantar fasciitis, Relatyv employs tailored treatment protocols based on three pillars:
Electroanalgesia leverages pulses of electrical current to stop pain signals traveling from the diseased area of your foot to the brain, thus providing long-lasting relief from pain. This therapy also promotes blood and oxygen circulation, stimulates the release of endorphins, and supports the healing of damaged tissues.
Unlike OTC electrical stimulation alternatives, electroanalgesia is able to deliver over 10,000 electrical pulses per second, which makes it a far superior and more efficient alternative.
Custom IV therapy plans are designed to address and correct nutritional deficiencies and imbalances that may be contributing to the inflammation, pain, and damage of your foot’s tissues.
Following comprehensive blood tests, a specialist at Relatyv will create an IV mix that contains all the essential nutrients, minerals, and vitamins needed to provide long-lasting hydration and support tissue regeneration.
An ad hoc Lifestyle Counseling journey is created to help you identify and modify those lifestyle choices that represent risk factors for chronic pain conditions, such as plantar fasciitis.
For example, if you are overweight or obese, deal with nutritional deficiencies, have a sedentary lifestyle, or have proinflammatory habits like smoking or drinking alcohol, you are at greater risk of high inflammation, circulatory problems, and chronic pain.
A lifestyle counselor at Relatyv can help you implement strategies to maintain a healthy weight, choose supportive shoes, start exercising regularly, and, ultimately, create a lifestyle that supports health in the long term.
Surgery for plantar fasciitis can condemn you to months or years of rehabilitation, immobilization, and physical therapy – and it is certainly not free of severe risks. So, before signing up for surgery, make sure you know all of your options and try the non-invasive alternatives offered at Relatyv.
Through Neurofunctional Pain Management, you can manage your pain, decrease inflammation, and regain your foot function without medications or surgery. So, you can return to enjoying your favorite activities and magnify your quality of life.
About the Author
Will is a healthcare executive, innovator, entrepreneur, inventor, and writer with a wide range of experience in the medical field. Will has multiple degrees in a wide range of subjects that give depth to his capability as an entrepreneur and capacity to operate as an innovative healthcare executive.
Share on Social Media
You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/
You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/
Neurofunctional Pain Management Overview
Symptoms
Conditions Treated
Treatments
Articles by Category
Locations
Colorado
Wisconsin
Georgia
Hiram
Lawrenceville
Marietta
Powder Springs
Texas
Waco
Victoria
Illinois
Buffalo Grove
New Lenox
St. Charles
Arizona
Tucson
Waddell
Arlington
Avondale
Buckeye
Superior
Mesa
Palo Verde
Morristown
Tempe
Chandler
Anthem
Eloy
Florence
Fort McDowell
Phoenix
El Mirage
Coolidge
Gilbert
Arizona City
Casa Grande
Casa Blanca
Aguila
Sacaton
Apache Junction
Kearny
Stanfield
Goodyear
Litchfield Park
Alabama
Arkansas
California
Florida
Idaho
Indiana
Iowa
Kansas
Louisiana
Maryland
Michigan
Rhode Island
Minnesota
Mississippi
Nevada
New Jersey
New Mexico
North Carolina
Ohio
Pennsylvania
South Dakota
Tennessee
Utah
Virginia
Washington


