Fibromyalgia

What Does Fibromyalgia Pain Feel Like?
Read More
August 30, 2023
Affecting 20 million and 4 million Americans respectively, neuropathy and fibromyalgia are among the most common pain conditions affecting adults of all ages. These disorders can lead to chronic widespread pain and cause severe limitations to your everyday personal and professional life.
But despite how common fibromyalgia and nerve pain are, a lot is yet to be understood about these conditions, including their causes and nature. Nonetheless, thanks to recent research, a connection between nerve dysfunction and fibromyalgia pain has started to emerge. In turn, these findings may open up the path to new, innovative treatment options for patients battling chronic pain.
In this guide, we’ll look at how the whole-person program developed by Relatyv – Neurofunctional Pain Management – targets the underlying causes of chronic pain and offers patients a non-invasive and non-drug therapeutic approach. Let’s get started.
To understand the connection between fibromyalgia and nerve pain, it is first important to clarify how these conditions are defined:
Given the “invisible” nature of fibromyalgia, this disorder remains difficult to diagnose and manage. What’s more, research is still ongoing to determine the nature and causes of this condition.
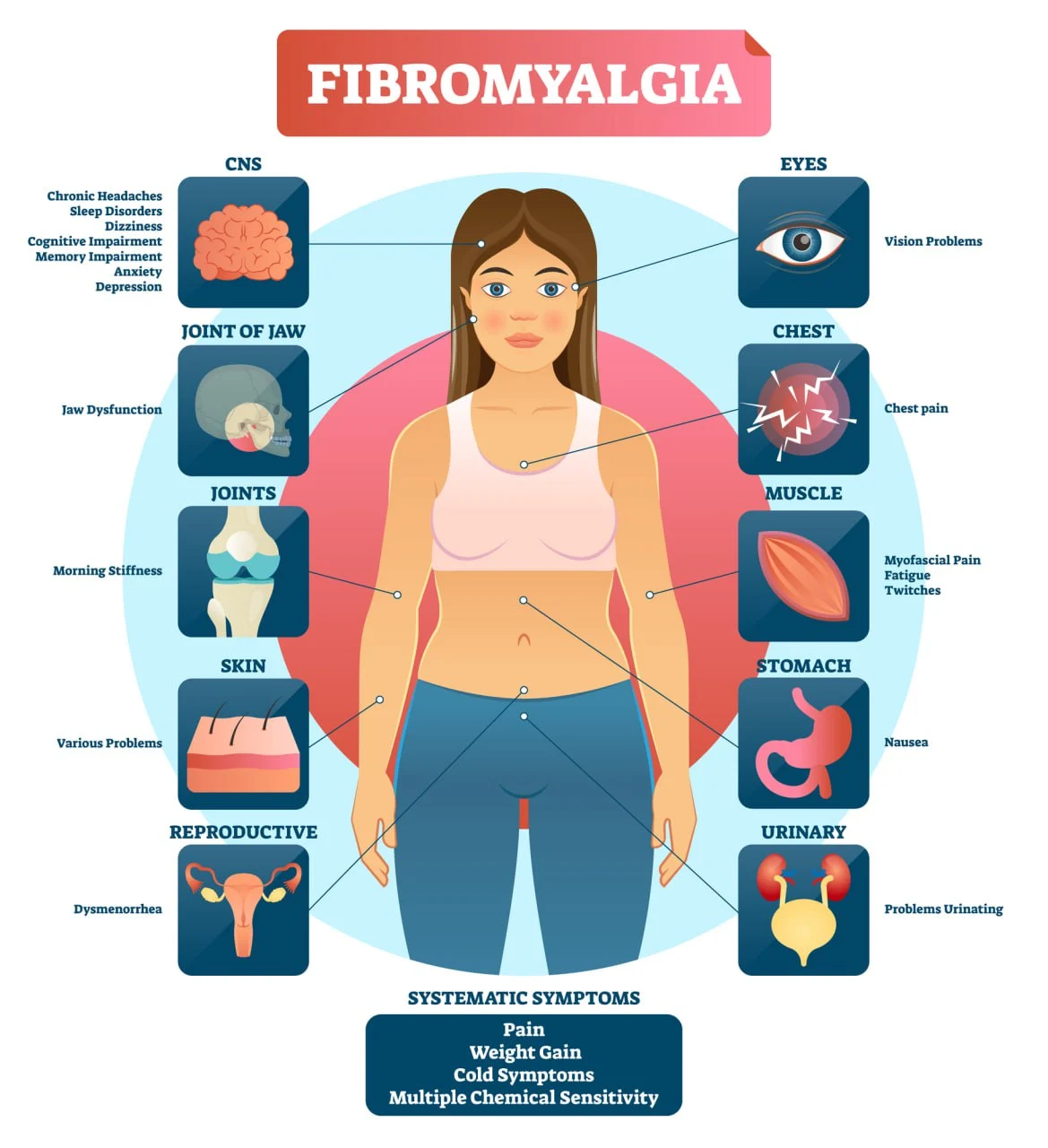
According to studies, fibromyalgia is linked to disturbances in the normal processing of pain signals deriving from dysfunction of the central nervous system, i.e. the brain or spinal cord. In turn, patients with fibromyalgia are more sensitive to pain or experience excessive pain in response to stimuli that should normally be painless or mildly uncomfortable.
People with fibromyalgia also tend to suffer from hypersensitivity to light, temperature, sounds, and smells, as well as difficulties with autonomic functions like increased sweating and irregular heartbeat. All of these are symptoms that can be traced back to altered neurological function.
It has also been seen that fibromyalgia is more likely to occur in people who suffer from nerve damage and pain. According to a 2019 study, nearly 50% of people with fibromyalgia also had small fiber pathology, which is a form of neuropathy that causes burning pain and prickling sensations.
Research conducted in 2014 on skin samples of people with and without fibromyalgia showed that those diagnosed with this condition have a much lower density of nerve fibers on the outer layer of the skin.
Other aspects that indicate that fibromyalgia may be neuropathic in nature include:
Although ongoing research shows even more similarities between the two conditions, the physiological changes that cause fibromyalgia (pathophysiology) are unclear. Because of this, according to a 2018 review, fibromyalgia does not meet the “current criteria for the definition of neuropathic pain.”
Below, we’ll look at the aspects that set fibromyalgia and neuropathy apart.
Although fibromyalgia and nerve pain may be interconnected and have overlapping symptoms, there are critical differences between these two conditions that are worth noting.
This knowledge can help you identify your symptoms correctly, facilitate an accurate diagnosis, and find an adequate management strategy as swiftly as possible.
One of the main similarities between fibromyalgia and nerve pain is that these two conditions cause pain throughout the body, often described as burning or prickling. Both disorders are also associated with numbness, tingling sensations, and excessive sensitivity to external stimuli.
However, a closer examination shows some differences.
Historically, according to the official guidelines published in 1990 by the American College of Rheumatology, fibromyalgia was diagnosed by examining 18 sites in the body. These sites included regions in the upper arm, the back of the shoulders, the upper edge of the breast, the knee, the leg, the hip bone, and the base of the skull.
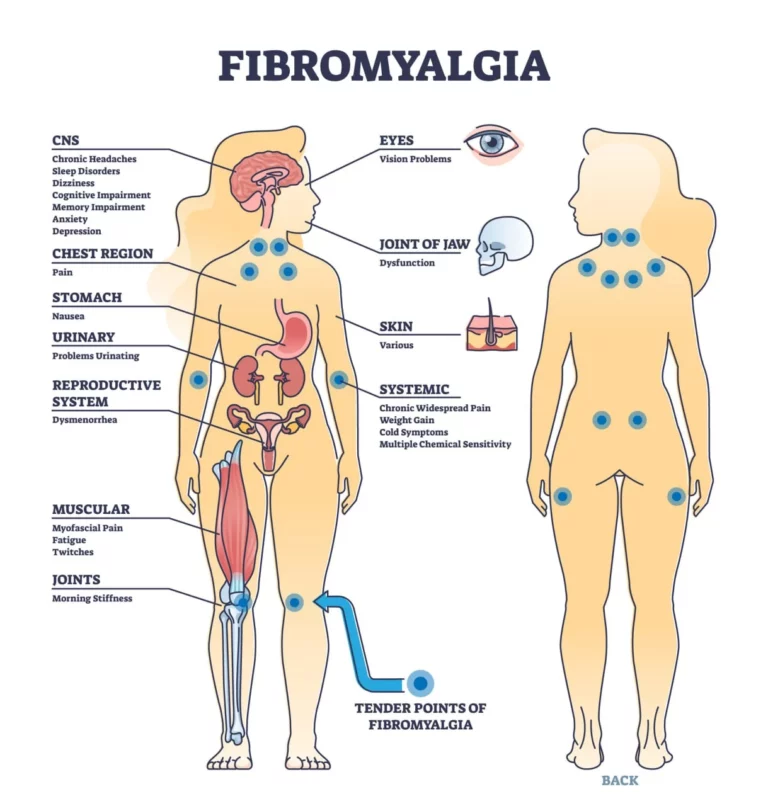
If, at the time of examination, patients experienced pain in at least 11 of these 18 “tender spots”, they were diagnosed with fibromyalgia. These diagnostic criteria were updated in 2010 following findings that show how the pain caused by fibromyalgia tends to move across the body and change in location and intensity over time.
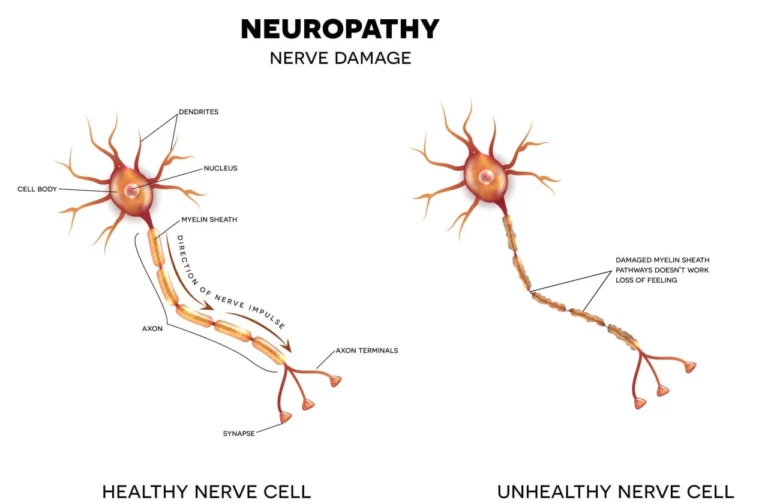
On the other hand, nerve pain caused by neuropathy follows what’s known as the “dying-back phenomenon” or axonal degeneration. This process dictates that the longer nerves, which are also those located the furthest from the brain and the spinal cord, are the first ones to be affected by degenerative damage. Thanks to this process, the more important nerves in the peripheral nervous system that connect to vital organs are protected for longer.
Because of the “dying-back phenomenon”, you’ll begin to experience pain, numbness, and extreme sensitivity to touch in the hands, fingers, feet, or toes. Over time, the pain can progress and start affecting your arms and legs before spreading across the body.
As we have seen above, the causes of fibromyalgia are unclear. Current hypotheses show that dysfunction of the nervous system may be involved. However, other studies present different theories.
For example, a 2020 study explored the connection between fibromyalgia and gut microbiome composition, while 2021 research links this pain condition to dysfunction of the immune system. What’s more, in most cases, the onset of fibromyalgia is associated with another major health event, such as a traumatic injury or mental health illness.
When looking at the causes of neuropathy, different patterns emerge. Nerve damage can be caused by several conditions, including:
It is important to note that up to 30% of cases of neuropathy are idiopathic, meaning that they have no known cause.
Until 2010, fibromyalgia used to be diagnosed through a physical examination, during which a doctor would gently press on the 18 tender spots of the body. However, following the updated diagnostic criteria published by the American College of Rheumatology in 2010, doctors now use a wide range of tools to diagnose this condition, including
When it comes down to diagnosing neuropathy, doctors will use similar tools to the ones seen above. However, they may also use electrodiagnostic tests, biopsies, and neurological examinations to determine the location, cause, and extent of nerve damage.
Imaging tests like CT and MRI scans may be recommended to ascertain the presence of anomalies (i.e. tumors) pressing on and damaging a certain nerve.
One of the aspects that makes fibromyalgia and neuropathy so difficult to diagnose and manage is that their symptoms are often similar or overlapping. Next, we’ll look at the most common telltale signs of these conditions.
Damage to nerve fibers or their protective sheath (myelin) interferes with the normal transmission of signals relating to pain, touch, temperature, and vibration. When your nerves are damaged or are unable to send these signals as they should, you may experience what’s known as paresthesia, or tingling and prickling sensations.
Paresthesia is also associated with other symptoms, including:
The inability to properly experience sensation can lead to severe complications. For example, if your toes are numb, you may inadvertently expose your feet to extreme heat or cold, or let an infected wound go untreated. When this happens, you may suffer tissue degeneration and ulcers which, in diabetic patients, account for up to 75% of nontraumatic limb amputations.
Muscle pain arises as a complication of nerve damage. When the nerves responsible for carrying motor signals to the brain are damaged, you may begin to experience involuntary muscle movements, painful cramps, and spasms.
As your disorder progresses, you may lose your ability to voluntarily move your muscles, which translates into balance and coordination problems, as well as the shrinking of the muscle mass.
What’s more, both fibromyalgia and neuropathy interfere with how your brain processes painful and non-painful signals, causing physical sensations to appear more intense.
Alongside widespread pain, chronic fatigue is one of the most debilitating aspects of both fibromyalgia and neuropathy. This symptom occurs due to the fact that damaged nerves are unable to support the contraction and relaxation of the blood vessels that supply muscles around the body. The difficulty of supplying muscles with enough oxygen and blood translates into an excessive drain of energy, which results in constant fatigue.
This symptom is also aggravated by chronic pain and the impact on mental health it can have. A 2020 study shows that, among those with neuropathy, 65.6% also suffered from depression, and 73.7% from anxiety disorders. In turn, these mental health disorders are known to cause persistent feelings of sadness, a lack of energy, sleep disturbances, and fatigue.
As we have seen above, both neuropathy and fibromyalgia cause increased sensitivity to touch. These painful sensations tend to become more noticeable at night when there are fewer distractions and external stimuli. In turn, for people with nerve pain, even the light brushing of the bed sheets on the skin can become excruciatingly painful.
The pain and discomfort you experience at nighttime can prevent you from falling asleep and staying asleep, which can impact your daytime productivity and increase your levels of fatigue and stress.
According to estimations, 70% of people with nerve damage experience sleep disturbances, and 96% of people with fibromyalgia are problem sleepers. Some of the most common sleep disorders affecting those diagnosed with neuropathy or chronic pain include insomnia, trouble falling asleep, and non-restorative sleep.
If neuropathy is often challenging to diagnose, fibromyalgia is even more so. According to 2018 estimations, patients tend to wait over six years to obtain an accurate diagnosis and, in most cases, the root cause of their chronic pain remains unknown.
Because of this, most treatment programs for fibromyalgia and nerve pain aim to help patients manage their symptoms, rather than target the underlying condition that is causing chronic pain.
Here are the shared treatment approaches for these two conditions, their benefits, and their limitations.
Medications are considered the go-to solution for patients struggling with widespread chronic pain. The most commonly used classes of drugs for chronic pain include:
It is important to note that both neuropathy and fibromyalgia are chronic conditions, which means that you’d need to take medications regularly to manage ongoing pain and distress.
But the side effects of this decision cannot be overlooked. The regular consumption of painkillers, antidepressants, antiepileptics, and opioids can lead to a cascade of side effects, including the increased risk of stroke and heart attack, ulcers, sleep disturbances, mood swings, and addiction.
Physical and occupational therapy play an important role in helping patients manage their chronic pain and adapt their lifestyle to prevent severe complications.
In particular, a review published in 2000 shows that physical therapy and regular cardiovascular fitness exercises can reduce pain, boost energy levels, and promote overall musculoskeletal health. It is also important to note that regular physical activity can improve muscle strength and flexibility, and help people fight the risk factors for both neuropathy and fibromyalgia, such as diabetes, obesity, and poor cardiovascular health.
Acupuncture, as well as other natural remedies like massages, meditation, and mind-body exercises (e.g. yoga), can have multiple beneficial effects. Firstly, acupuncture has been seen to induce an overall sense of well-being and trigger the release of endorphins, the body’s natural painkilling hormones.
Additionally, these therapies can help relax tense muscles, which prevents painful spasms and cramps. Lastly, massages can support the circulation of blood and oxygen around the damaged nerve endings, thus preventing further damage.
While these therapies may help people with chronic pain, they don’t work equally well for all patients, and results may only be temporary.
Possible internal link to “TENS Unit For Neuropathy – Is It Your Best Treatment Option?”
TENS – or transcutaneous electrical nerve stimulation – refers to a therapy that involves targeting a painful area with low-frequency electrical pulses. The electrical current has a similar effect to the one of acupuncture: it may help relax tense muscles, alleviate pain, and support blood and oxygen circulation around the areas affected by pain.
TENS units are available as an over-the-counter solution and, given that they are only able to deliver low-frequency pulses, they are considered generally safe. However, the relief this therapy provides is only limited to the duration of the treatment and cannot be considered a long-term solution.
Although a lot is yet to be understood about the connection between fibromyalgia and neuropathic pain, one aspect is certain: most treatments prescribed for these conditions are inefficient at best and harmful at worst.
Fortunately, taking medications daily to ease your pain or facing the prospect of living with your condition for years to come are no longer the only options. Thanks to the innovative treatment program pioneered by Relatyv, you can target the underlying cause of your chronic pain, prevent complications, ease discomfort, and, ultimately, magnify your quality of life.
Neurofunctional Pain Management is a whole-person approach that aims to target all of those lifestyle and health factors that contribute to or aggravate your chronic pain. Thanks to non-invasive, non-drug, and non-chiropractic therapies, this customized treatment program can help you make positive changes, understand the nature of your conditions, and build the foundations of long-term health.

Some of the key pillars of Neurofunctional Pain Management are:
Obtaining a diagnosis of fibromyalgia or neuropathy can be a life-changing moment, especially when facing the prospect of not being able to access an efficient treatment program for your condition. Fortunately, this is no longer the case.
With Neurofunctional Pain Management, you can start working towards a pain-free, healthy life – without medications or surgery.
About the Author
Will is a healthcare executive, innovator, entrepreneur, inventor, and writer with a wide range of experience in the medical field. Will has multiple degrees in a wide range of subjects that give depth to his capability as an entrepreneur and capacity to operate as an innovative healthcare executive.
Share on Social Media
You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/
You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/
Neurofunctional Pain Management Overview
Symptoms
Conditions Treated
Treatments
Articles by Category
Locations
Colorado
Wisconsin
Georgia
Hiram
Lawrenceville
Marietta
Powder Springs
Texas
Waco
Victoria
Illinois
Buffalo Grove
New Lenox
St. Charles
Arizona
Tucson
Waddell
Arlington
Avondale
Buckeye
Superior
Mesa
Palo Verde
Morristown
Tempe
Chandler
Anthem
Eloy
Florence
Fort McDowell
Phoenix
El Mirage
Coolidge
Gilbert
Arizona City
Casa Grande
Casa Blanca
Aguila
Sacaton
Apache Junction
Kearny
Stanfield
Goodyear
Litchfield Park
Alabama
Arkansas
California
Florida
Idaho
Indiana
Iowa
Kansas
Louisiana
Maryland
Michigan
Rhode Island
Minnesota
Mississippi
Nevada
New Jersey
New Mexico
North Carolina
Ohio
Pennsylvania
South Dakota
Tennessee
Utah
Virginia
Washington

