Chronic Fatigue Syndrome

Different Chronic Fatigue Syndrome Treatments
Read More
August 14, 2023
Feeling low on energy after strenuous physical activity or following an intense week at work is something we all experience. But when the tiredness and weakness become persistent or don’t improve with rest, it is important not to overlook your symptoms.
Over time, chronic fatigue can compromise your productivity, social life, and ability to live independently. However, there is no need to just surrender to fatigue: there are many treatment options available that can help you boost your energy levels and return to your true self.
In this guide, we’ll explore how the innovative whole-person treatment program pioneered by Relatyv, Neurofunctional Pain Management, can help you defeat chronic fatigue without medications, chiropractic therapies, or invasive procedures. Let’s dive in.
Chronic fatigue – officially known as myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) – is a chronic disorder that causes a persistent state of fatigue for at least six months.
If you have CFS, rest and sleep won’t help your symptoms, which will continue to grow in intensity and severity over time, ultimately getting in the way of your professional and personal lives.
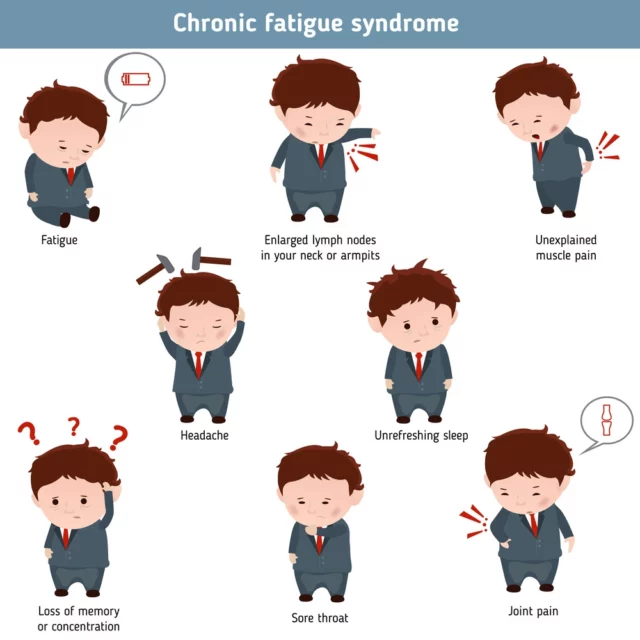
Some of the common symptoms of CFS include:
These symptoms tend to get worse after spending a long time on your feet, or the day after intense physical activity. This is a complication of CFS known as post-exertional malaise.
The causes of chronic fatigue syndrome are unknown. However, new studies have found links between this condition and certain anomalies, such as:
While the root cause of chronic fatigue syndrome isn’t clearly determined, some factors have been seen to increase the risk of developing this disorder. These risk factors include:
Currently, between 0.4% and 2.5% of the general population has been diagnosed with chronic fatigue syndrome, and these rates are steadily growing. However, it is estimated that the actual number of Americans battling CFS is much higher, sitting somewhere between 836,000 to 2.5 million – 90% of whom have not yet been diagnosed.
One of the aspects that make chronic fatigue syndrome so hard to diagnose is that its symptoms tend to overlap those of several other diseases. Below, we’ll look at the conditions that also cause long-lasting tiredness, weakness, nausea, dizziness, and prolonged low levels of energy.
Affecting over four million people in America alone, fibromyalgia is a common condition that causes widespread musculoskeletal pain, distress, and muscle weakness. The constant pain and extreme sensitivity to touch also lead people with fibromyalgia to experience symptoms such as sleep disturbances, long-lasting fatigue, and impaired cognitive abilities.

The root causes of this condition are not well understood. However, new studies have highlighted that fibromyalgia may stem from dysfunctions of the immune system or of the central nervous system, which makes people more sensitive to pain. Additionally, similarities with certain autoimmune disorders may be opening up new pathways to better understand fibromyalgia.
Irritable bowel syndrome – or IBS – is a disorder that affects the part of the digestive system that involves the stomach and intestine. This is known as the gastrointestinal tract, and it plays a major role in enabling the digestion process.
As a form of functional gastrointestinal disorder, IBS occurs when there are anomalies in the gut-brain axis, i.e. the channel of communication between the central nervous system and the digestive system. When this happens, you may experience a range of symptoms associated with dysfunctions in the digestive process, including bloating, vomiting, diarrhea, constipation, and changes in bowel movements.
These symptoms tend to last between a few days and a few weeks, and, over time, they can impact your body’s ability to obtain essential nutrients from food. The lack of vitamins and minerals, coupled with the dehydration derived from recurring diarrhea, can cause severe complications such as fatigue, muscle weakness, dizziness, and low levels of energy.
Clinical depression – or major depressive disorder – is a psychological disorder that impacts the mood, as well as how you feel or behave. It causes persistent feelings of sadness, hopelessness, and emptiness, as well as anger, frustration, irritability, and loss of interest and pleasure in activities.
The emotional disturbances caused by clinical depression can cause a whole host of severe complications, including physical problems, difficulty living independently, and suicidal thoughts. People with depression can also experience severe sleep disturbances and sleep disorders like insomnia, as well as impaired cognitive function and memory problems.
The combination of all of these symptoms can also cause people with depression to experience persistent fatigue, tiredness, and weakness. Currently, it is estimated that depression affects over 280 million people worldwide.

If you have been struggling with persistent fatigue, you should immediately seek an accurate diagnosis. Currently, there is no single, specific test that your doctor can prescribe to diagnose CFS.
However, depending on your symptoms, your healthcare provider may use a range of tests and examinations to deliver an accurate diagnosis. This step is essential for two main reasons:
Besides a review of your symptoms and medical history, your doctor may carry out a physical exam and prescribe imaging tests to rule out fatigue-inducing anomalies (for example, diseases like tumors and cancers can cause “cancer fatigue”).
Seeking a diagnosis as soon as your symptoms seem to be persistent or recurring can help you find an efficient treatment program that allows you to manage your symptoms and treat their underlying cause.
Below, we’ll look at the most common lines of treatment prescribed for CFS – or symptoms that involve chronic fatigue.
Some lifestyle changes may help improve your levels of energy and counteract the effects of chronic fatigue syndrome. These include:
Foods such as vegetables, legumes, whole grains, nuts, and seeds provide a wealth of health benefits and can help you avoid nutritional deficiencies that are linked to fatigue, impaired cognition, and weakness (e.g. iron, vitamin B12, and vitamin D).
Changing your workplace, school, or routine can help you gain more control over your surrounding environment and ease the symptoms of CFS.
To lower your stress levels, you may try tools such as regular light exercise, meditation, breathing exercises, and mind-body activities such as yoga and Qigong.
Medications and supplements are often used alongside lifestyle modifications to help patients manage the symptoms of CFS in their daily lives. We’ll look at the different lines of treatment, their benefits, and their limitations.
Medications can help people with CFS by helping them enjoy a better night’s sleep, feel more alert during the daytime, relieve environmental stressors (e.g. allergies), or address underlying conditions such as depression.
Commonly prescribed medications for CFS include:
It is important to note that these medications may only relieve temporary flare-ups, but they don’t treat or modify the underlying condition causing fatigue. What’s more, as we have seen above, CFS is a chronic condition that persists over time.
Taking medications for such long periods of time may expose you to severe side effects, including the increased risk of heart attack, stomach ulcer, kidney dysfunction, mood changes, and addiction.
Some vitamins and supplements may help reduce fatigue. These include:
Low levels of L-carnitine are associated with decreased brain and heart function, impaired muscle movement, and liver problems as well as tiredness and fatigue. L-carnitine supplements can help your body produce more energy.
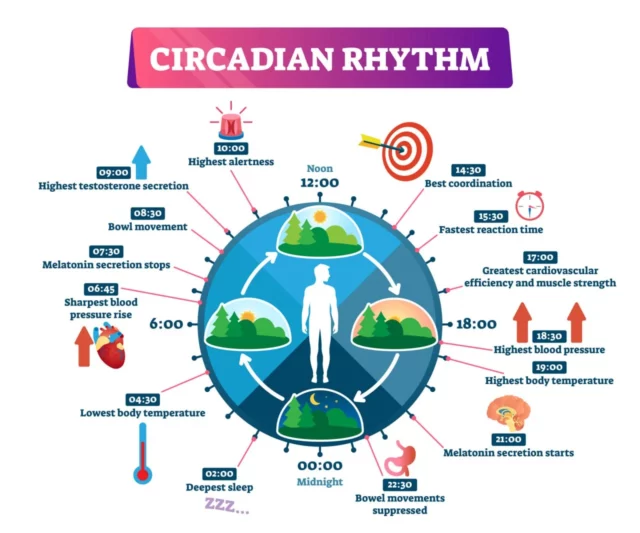
Other vitamins that may relieve fatigue include beta-carotene, which strengthens the immune system, and melatonin, which helps regulate the wake-sleep cycle and improve sleep quality. According to a review published in 2017, more research is needed to determine the efficacy of supplements on CFS.
Each of the supplements above comes with side effects and contraindications that should not be overlooked. Make sure to talk to your doctor before implementing them into your diet.
Herbal products have been used for centuries as part of traditional medicine. However, over the past three decades, the portion of people using herbs and herbal supplements as part of their primary healthcare has grown to 80%.
While research on the effects of herbs on chronic fatigue syndrome is still limited, some supplements may help with fatigue and weakness. These include Panax ginseng, a herb often used in traditional Chinese medicine.
Also known as ginseng, this herb may boost energy levels, regulate blood sugar, lower cholesterol levels, and promote relaxation. A 2022 study shows that out of 18 participants with CFS who were taking ginseng, 56% reported a significant improvement in their symptoms.

Other herbs and essential oils that may help with the symptoms of CFS by promoting relaxation, strengthening the immune system, or fighting oxidative stress include:
Although not all herbs are equally efficient, they can interfere with other medications you may be taking or even aggravate your sense of fatigue. Make sure to take these supplements only under the supervision of a medical practitioner.
If the lines of treatment above have failed, you and your doctor may discuss a different approach. Although there is no single therapy that works equally well for everyone, a combination of options can relieve your symptoms, strengthen your body, and help you learn how to live with your condition.
Here are some of the most common treatments for chronic fatigue syndrome.
Physical therapy – when combined with a custom exercise routine – can help you build muscle strength and endurance. Physical activity also offers some fringe benefits that should not be overlooked by those battling persistent fatigue:
Alongside physical therapy, other therapies that may help reduce stress, increase relaxation, and ultimately reduce fatigue include acupuncture and therapeutic massages.
Activity and energy management is an approach that aims to help you regulate your expenditure of energy during the day, so as to avoid excessive peaks and drops of energy. Complementing this approach, our energy IV therapy can provide a direct infusion of essential nutrients to support sustained vitality. The goal of this therapy, which is sometimes referred to as “pacing”, is to teach you how to maintain steady levels of activity throughout the day.
When implementing energy management strategies, you’ll strive to:
Although energy management plans may not cure chronic fatigue syndrome, they can help you manage your condition in the long term.
Cognitive behavioral therapy (CBT) is a form of talk or psychotherapy, often administered by a mental health counselor. During each session, your counselor will help you identify patterns in the way you think and analyze how you respond to specific situations. Over time, this can help you gain better control over the way you handle different circumstances and challenges.
CBT can also be used in the treatment of chronic fatigue. In this approach, you’ll work with a counselor over several weeks. In each session, you’ll learn to modify beliefs and thought processes that may be impairing your recovery, and you’ll also learn coping mechanisms and relaxation techniques.
According to a 2021 study published in Frontiers, a 16-week CBT program improves physical function and fatigue in people with mild to moderate chronic fatigue syndrome.
Chronic fatigue does a lot more than just make you feel tired. Over time, this condition can profoundly impact your life, making it harder to enjoy even the simplest of daily activities, such as going to work, taking care of your loved ones, or meeting your friends.
To make things worse is the fact that, with current traditional treatments, there is little chance of fully reversing chronic fatigue. And, as we have seen above, most therapies focus on simply relieving symptoms and offering coping strategies rather than tackling the roots of the problem.
Fortunately, thanks to the innovative approach pioneered by Relatyv, this is no longer the case. Neurofunctional Pain Management is a whole-person, non-pharmaceutical, and non-chiropractic treatment program that allows you to identify and change all of those aspects of your lifestyle and health that are aggravating your sense of fatigue.
Through a combination of the therapies below, Neurofunctional Pain Management can support your journey toward living free of persistent fatigue. Let’s see how.
Harnessing the power of high-frequency electric pulses, electroanalgesia stimulates the circulation of blood and nutrients, which are needed to support the body’s healing capabilities. The electric pulses delivered to the areas experiencing pain also disrupt the normal transmission of pain signals to the brain, thus providing long-lasting relief from pain.
What’s more, the massage-like feelings induced during each session of electroanalgesia stimulate the production of feel-good chemicals like endorphins and decrease stress hormone levels.
Following comprehensive blood tests and examinations, the expert team at Relatyv can help you identify and address those nutritional imbalances and deficiencies that may be contributing to your persistent fatigue.
Through a custom-designed course of IV mixes, you’ll be able to maintain appropriate levels of essential vitamins and minerals and provide your body with long-lasting hydration – which plays a vital role in restoring high levels of energy and liveliness.
As seen above, your habits and lifestyle choices have a significant impact on your levels of energy and fatigue. However, understanding how to change your lifestyle to promote health can be challenging.
With the guidance of the specialists at Relatyv, you can identify and change those lifestyle aspects that may be aggravating your feelings of fatigue – from exercise levels to environmental factors and dietary choices.
Chronic fatigue syndrome is a real and debilitating condition. However, thanks to the innovative treatment program introduced by Relatyv, there is no reason why you should just surrender to chronic fatigue.
A custom Neurofunctional Pain Management program designed around your unique needs can help you defeat fatigue and return to enjoy your life to the fullest.
About the Author
Will is a healthcare executive, innovator, entrepreneur, inventor, and writer with a wide range of experience in the medical field. Will has multiple degrees in a wide range of subjects that give depth to his capability as an entrepreneur and capacity to operate as an innovative healthcare executive.
Share on Social Media


You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/
You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/
Neurofunctional Pain Management Overview
IV Therapy
Symptoms
Conditions Treated
Treatments
Articles by Category
Locations
Colorado
Wisconsin
Georgia
Hiram
Lawrenceville
Marietta
Powder Springs
Texas
Waco
Victoria
Illinois
Buffalo Grove
New Lenox
St. Charles
Arizona
Tucson
Waddell
Arlington
Avondale
Buckeye
Superior
Mesa
Palo Verde
Morristown
Tempe
Chandler
Anthem
Eloy
Florence
Fort McDowell
Phoenix
El Mirage
Coolidge
Gilbert
Arizona City
Casa Grande
Casa Blanca
Aguila
Sacaton
Apache Junction
Kearny
Stanfield
Goodyear
Litchfield Park
Alabama
Arkansas
California
Florida
Idaho
Michigan
Rhode Island
Minnesota
New Mexico
North Carolina
Ohio
Pennsylvania
South Dakota
Tennessee
Virginia

