Over 1.3 million people in the US alone are affected by rheumatoid arthritis (RA), making this disease one of the leading causes of chronic pain and disability in the country. Learn more about our RA treatment options. Being diagnosed with RA can have a wide range of profound consequences on a person’s life.
Up to 30% of patients become permanently work-disabled within the first two to three years of the disease, while 41% and 11% experience activity and social limitations, respectively.
For many, what is truly unbearable about receiving a diagnosis of RA is the fact that this condition has no cure. This means that, often, the only treatment options are medications, doubtful complementary therapies, and, eventually, surgery.
Over time, the side effects of surgery, increased disability, and the prospect of having to undergo surgery can take a toll on a person’s mental health. It isn’t surprising that up to 48% of people with RA suffer from some form of depression.
Fortunately, thanks to the state-of-the-art approach pioneered by RELATYV Mobile Pain Management, being diagnosed with RA is no longer a sentence to living half a life. Beyond simply easing your symptoms, Neurofunctional Pain Management tackles the systemic inflammation at the root of rheumatoid arthritis without drugs or invasive procedures, allowing you to build the foundations of long-term health and magnifying your quality of life.
Let’s explore how this revolutionary method works below.
What Is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is a type of inflammatory arthritis, an autoimmune disease that occurs when the body’s immune system mistakenly attacks healthy tissues. This lifelong condition causes pain and stiffness in several joints across the body and, if left untreated, it can lead to permanent joint damage and disability.
To better understand what RA is and how it develops, let’s start by looking at how healthy joints work.
A joint is where two or more bones meet. Its role is to enable movement while controlling how far and in what directions the different bones and muscles move.
Thanks to the complex structure of connective tissues (i.e. tendons and ligaments) and cartilage, the joints across the body are able to prevent injuries – such as bones slipping out of place – and allow for everyday activities from walking and running to grasping objects and performing sports.
There are different types of joints in the body, but the most common one is a synovial joint. Synovial joints include the knee, hip, and shoulders, and are characterized by certain features:
- Strong bands of connective tissues – the ligaments and tendons – connect the bones and to the surrounding muscles. Their role is to prevent injuries and regulate the joint’s range of movement.
- The end of each bone is cushioned by a slippery disc of gel-like fluid, known as articular cartilage, which allows the bones to glide easily across one another during movement.
- The joint is encapsulated in a thin lining of tissue called synovium. This membrane produces hyaluronic acid and other substances that help keep the joint lubricated and protected from shock.
- Synovial tissue, called tenosynovium, lines the tight tunnels where the tendons run, to protect them from friction damage and allow them to glide within the tunnels.
Rheumatoid arthritis occurs when certain cells of the immune system begin to mistakenly attack healthy tissues in the body, especially the synovial tissue and the tenosynovium.
The malfunctioning immune cells begin to release substances that cause inflammation in the synovium, which causes it to swell and thicken. The inflammatory cells also begin to spread across surrounding tissues, including the cartilage and bones. When the tenosynovium is affected, the tendon sheaths (which are the tunnels that house the tendons) become swollen and cause damage to the tendons, leading to severe tendon tears.
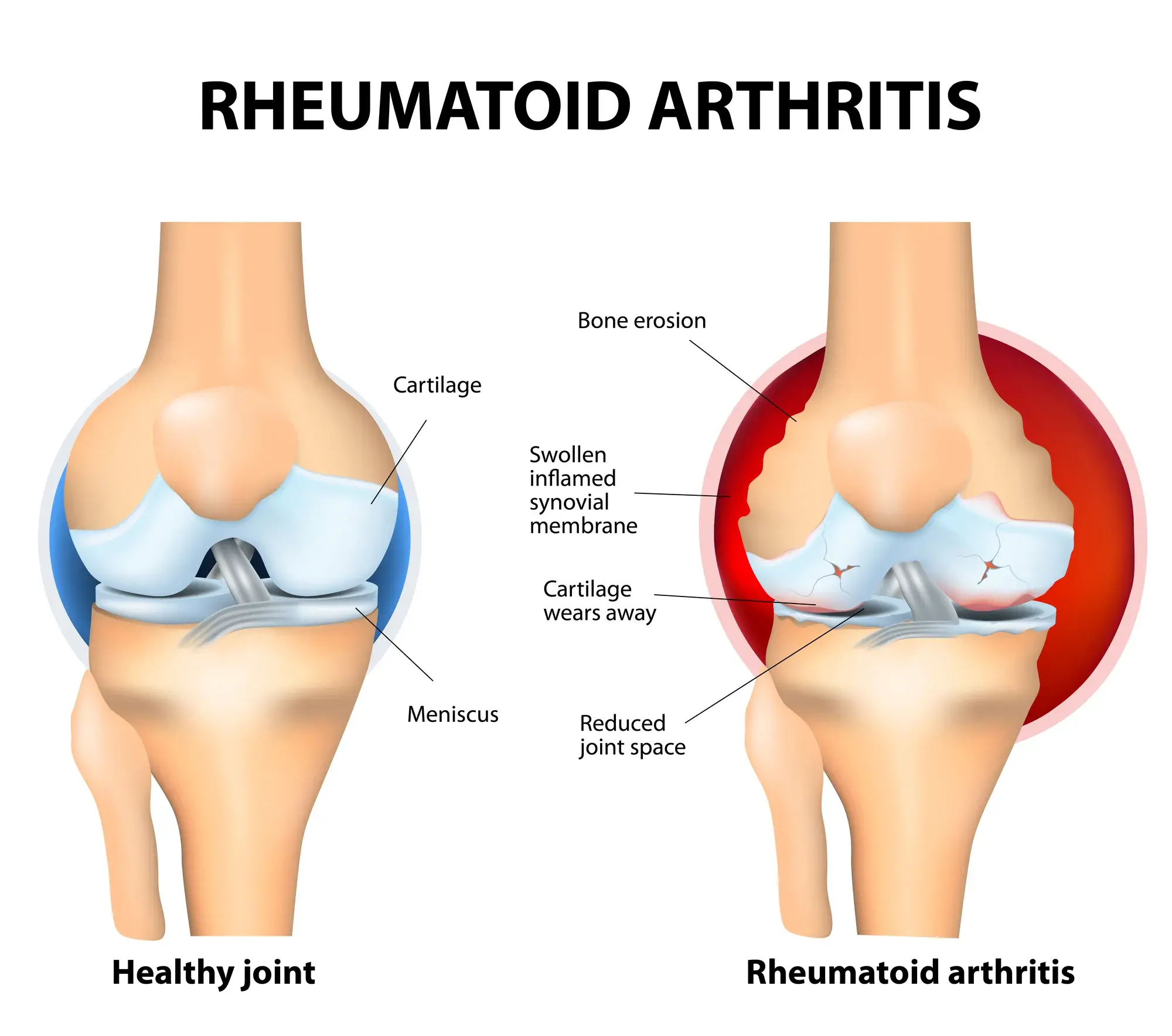
Besides pain, stiffness, and reduced range of motion, if left untreated, RA can also lead to permanent joint damage and serious disability. However, thanks to advanced treatment options, it is now possible to modify the disease, prevent the progression of joint damage, and avoid the most serious complications of RA, including deformities and joint destruction.
What Are The Symptoms Of Rheumatoid Arthritis?
The symptoms of rheumatoid arthritis vary greatly, depending on how advanced the disease is and what joints are affected. However, most people with this condition report the following symptoms:
- Pain around and radiating from the joint affected
- Joints that ache even when at rest
- Joint swelling, redness, and warmth, are the consequences of inflammation
- Stiffness, especially after periods of rest (in the mornings or after sitting for a long time)
- Symptoms that spread across the body, such as fever, low energy levels, and loss of appetite
- Complications of inflammation, including dry eyes and chest pain
- Fatigue and weakness, often due to low levels of red blood cells (anemia)
- Deformities and contractures (the stiffening and shortening of tissues in the joint), such as bunions and hammer toes
- Nodules or fleshy lumps – known as rheumatoid nodules – which are present in up to 25% of people with RA.
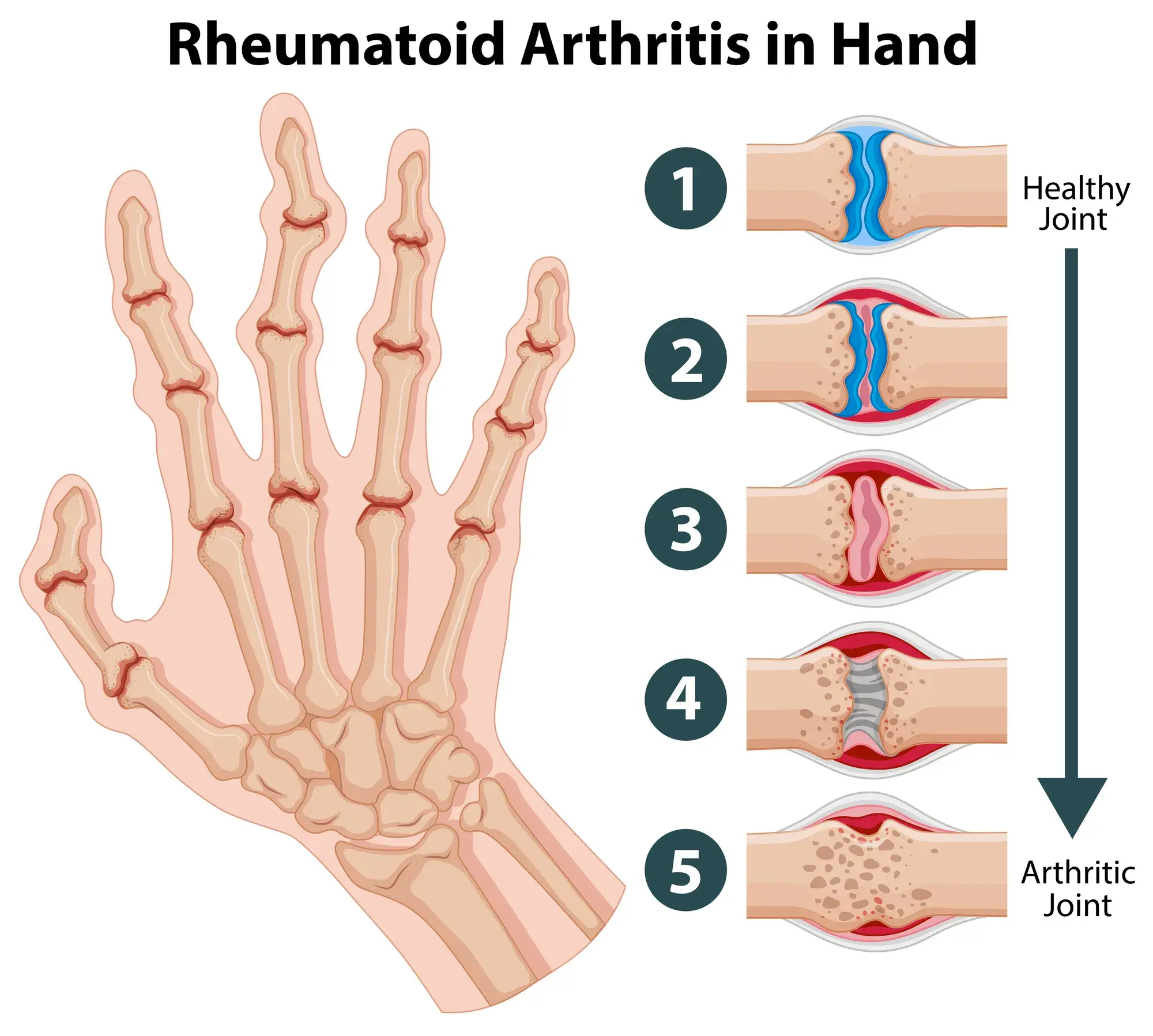
The joints most commonly affected by RA are fingers, hands, wrists, knees, ankles, feet, and toes. The early symptoms of RA are most commonly felt in the smallest joints of the fingers and toes, and they usually affect the same joint on both sides of the body (e.g. both hands or both feet).
The intensity of symptoms tends to increase alongside the progression of the disease, but it significantly increases during flare-ups. Studies show that over 23% of people with RA experience sustained remission (months or years without symptoms) without medications. Others notice that their symptoms come and go, and they are only noticeable during flare-ups.
Nonetheless, even during periods of remission, these people aren’t cured. Uncontrolled inflammation can, over time, lead to a wide range of impactful symptoms, including pains in different areas of the body, weakness, spasms, and disability. We’ll look at these symptoms in more detail below.
What Causes RA?
The exact cause of RA is unknown. However, researchers have unveiled that certain environmental factors may act as triggers, which activate the disease in people who carry certain genes. Even though RA isn’t considered an inherited disease, when the body is exposed to these triggers, the immune system begins to respond incorrectly, leading to rheumatoid arthritis.
There are several known triggers for RA, and they may vary from one person to another. However, the most common ones include:
- Genetics. While it is unclear what the genetic correlation to RA is, it has been seen that triggers such as smoking and diet can lead to the development of disease in people who have a certain genetic makeup. In particular, having the HLA gene sequences can increase the risk of RA five-fold.
Other genes linked with RA include PTPN22, STAT4, TRAF1, and C5, which are associated with the activation of the immune system and chronic inflammation. Additionally, having a relative with this condition can increase the risk.
- Hormones. Abnormal levels of certain hormones, especially corticosteroids and female sex hormones like estrogen and progesterone, have been seen to be associated with a higher risk of RA. This link may also contribute to the fact that females are two to three times more likely to develop this disease than males.
Similarly, the increase of estrogen and progesterone levels during pregnancy may prevent the onset or flare-ups of RA.
- Infection. When you suffer an infection, your immune system activates to fight it off. As it triggers inflammation, the inflammatory response can continue developing uncontrolled and lead to the development of RA.
This is more likely in people with strong immune systems or higher levels of antibodies. Infections that may act as triggers for arthritis include mononucleosis (Epstein-Barr virus).
- Smoking. Cigarette smoking is one of the leading triggers for RA. After receiving an AR diagnosis, smoking can also cause worse symptoms (compared to non-smoking patients) and weaken the effects of medications.
Although the risk of RA decreases over time after quitting smoking, former smokers are still at higher risk than those who never smoked, even 15 years after quitting.
- Physical and emotional stress. Experiencing stress prompts your body to produce substances that may trigger inflammatory reactions. When occasional, stress is a normal part of life. However, when high-stress levels become chronic, these can increase the risk of a wide range of inflammatory diseases, including RA. To address chronic stress, consider trying out meditation and breathing exercises, or opting for therapy.
There are also other known triggers to RA, including trauma, pollutants, obesity, medication issues, overexertion, sleep problems, being physically inactive, and even certain weather events. While there’s a lot yet to be understood about the link between these trigger factors and RA, most of them affect the body’s immune response and systemic inflammation in one way or another.
Who Is At Risk For RA?
Since the cause of RA isn’t well understood, it can be challenging to identify who is likely to be at greater risk of this disease. However, there are some known risk factors worth being aware of. These include:
- Age. RA can affect anyone, at any age. However, diagnosis is more common between the ages of 30 and 60. Younger people, especially children and adolescents, may also develop a form of RA known as juvenile idiopathic arthritis (JIA), which differs in several ways from rheumatoid arthritis in adults.
Three-quarters of people with arthritis are within their working age when they are first diagnosed.
- Gender. Women are two to three times more likely than men to develop RA. This is due to a wide range of reasons, including abnormal levels of female sex hormones (progesterone and estrogen) and a typically stronger immune system.
Studies are also unveiling how autoimmunity is under genetic control and, in turn, under the control of the genes in sex chromosomes. This makes women more prone to developing autoimmune diseases.
- Heredity. Although RA isn’t an inherited disease, people with a close relative with rheumatoid arthritis are at greater risk of developing this condition. Having a first-degree relative with RA increases the risk five-fold compared to the general population.
- Weight. Obese and overweight patients (those with a high body mass index) are more likely to develop RA. This is because the excess fat stored in the body produces cytokines, which are inflammatory proteins. If you are obese and have RA, your symptoms may be more intense, inflammation levels greater, and medications less effective.
- Joint injury. When you suffer a joint injury, such as a fracture or dislocation, your body will trigger an inflammatory response, which can become chronic. This can lead to the spread of inflammation to surrounding components of the joint, which can initiate RA.
- Infection. As we have seen above, the inflammatory response triggered to combat an infection can develop into chronic, uncontrolled inflammation, which can trigger RA.
These risk factors tend to act as triggers in individuals with a genetic propensity toward rheumatoid arthritis, such as testing positive for the rheumatoid factor or antinuclear antibody test. We’ll look into these aspects later on in this guide.
Possible Complications Of RA When Left Untreated
As we have seen above, the latest advancements in research are now helping patients avoid the most devastating complications of RA and prevent the progression of this disease. Nonetheless, if left unaddressed, the uncontrolled inflammation that fuels rheumatoid arthritis can lead to the emergence of a wide range of severe complications.
Below, we’ll look at the most common conditions that occur when RA – and its underlying systemic inflammation – are left untreated.
Osteoporosis
Osteoporosis is a condition characterized by the loss of bone mass and mineral density, thus leading to fragile, porous bones. This brittleness happens due to an imbalance in the body’s mechanism of forming new bone and reabsorbing old bone: in people with osteoporosis, bone mass is lost at a faster rate than it is regenerated.
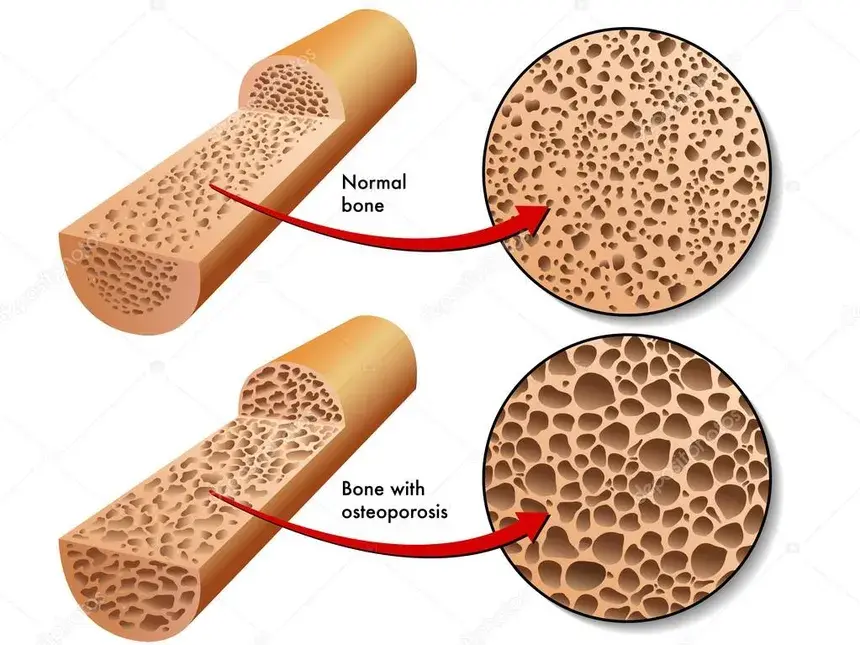
Common risk factors for osteoporosis include age, family history, menopause, low body weight, and lifestyle habits like smoking and alcohol abuse. Because of these risk factors, the demographics at risk include postmenopausal women and those with a family history of osteoporosis.
Osteoporosis is considered to be an “invisible” illness – you may not notice that you have it until you experience a fracture or undergo a screening test. The most common bones fractured by people with osteoporosis include the hip, wrist, or spinal bones (vertebrae).
Osteoporosis is different from arthritis, but the two conditions may be interrelated. RA, especially if untreated, causes increased bone loss and higher osteoporosis risks. This happens because the inflammatory process enhances bone erosion and causes large cysts around the joints.
Both factors can contribute to a decline in the mineral content of the bone. Studies show that nearly 30% of people with RA have low bone mass density (osteopenia) or osteoporosis.
Rheumatoid Nodules
Rheumatoid nodules are firm lumps that often form under the skin near joints affected by RA. They can range in size – from pea-sized to golf ball-sized – and typically aren’t painful, unless they enlarge and begin to press on nearby nerves.
Given that they are a consequence of the high levels of uncontrolled inflammation, the emergence of rheumatoid nodules goes hand-in-hand with the progression of the disease. They are more likely in people who have high levels of rheumatoid factor or have had the disease for a longer period. Smoking and certain RA medications, like methotrexate and anti-TNF drugs, can also increase this risk of rheumatoid nodules.
The most common joints affected by rheumatoid nodules include the elbows, fingers, and knuckles, but they can appear on or around any joint affected by RA. This complication of RA can be effectively managed – and, in some cases, prevented – through a timely diagnosis and appropriate treatment. Historically, around 30% of people with RA developed this complication – however, the incidence of rheumatoid nodules has decreased substantially over time.
Sjogren’s Syndrome
Sjogren’s syndrome is an autoimmune disorder characterized by the malfunctioning of the immune system, which begins to attack the glands that produce moisture. It primarily targets the moisture-producing glands in the eyes and mouth. While the exact cause of this condition is still debated, research has shown that contributing factors may include environmental and genetic triggers.
Nonetheless, there are some risk factors that have been associated with a greater chance of developing Sjogren’s syndrome. These include being female (due to the propensity to autoimmune disorders) and being aged 40 and over. Symptoms of this syndrome vary widely but usually include dry eyes and mouth, joint pain, and fatigue.
People with rheumatoid arthritis stand a significantly heightened risk of also developing this condition. It is estimated that up to 31% of people with RA show signs of Sjogren’s syndrome. This is because the dysfunction of the immune system present in people with RA paves the way for other autoimmune disorders, including Sjogren’s syndrome.
Carpal Tunnel Syndrome
Carpal tunnel syndrome (CTS) is a progressively painful condition of the hand and fingers that occurs due to the compression of the median nerve as it traverses the carpal tunnel – a passageway in the wrist formed by the carpal bones and ligaments.
This nerve is responsible for innervating and providing sensation to your thumb and most fingers, excluding the little finger. As the carpal tunnel narrows, the median nerve can become entrapped, inflamed, compressed, or inflamed, which can interfere with the normal transmission of nerve signals relating to sensation and movement. This can lead to problems with moving your hand and fingers, pain, numbness, and tingling sensations.
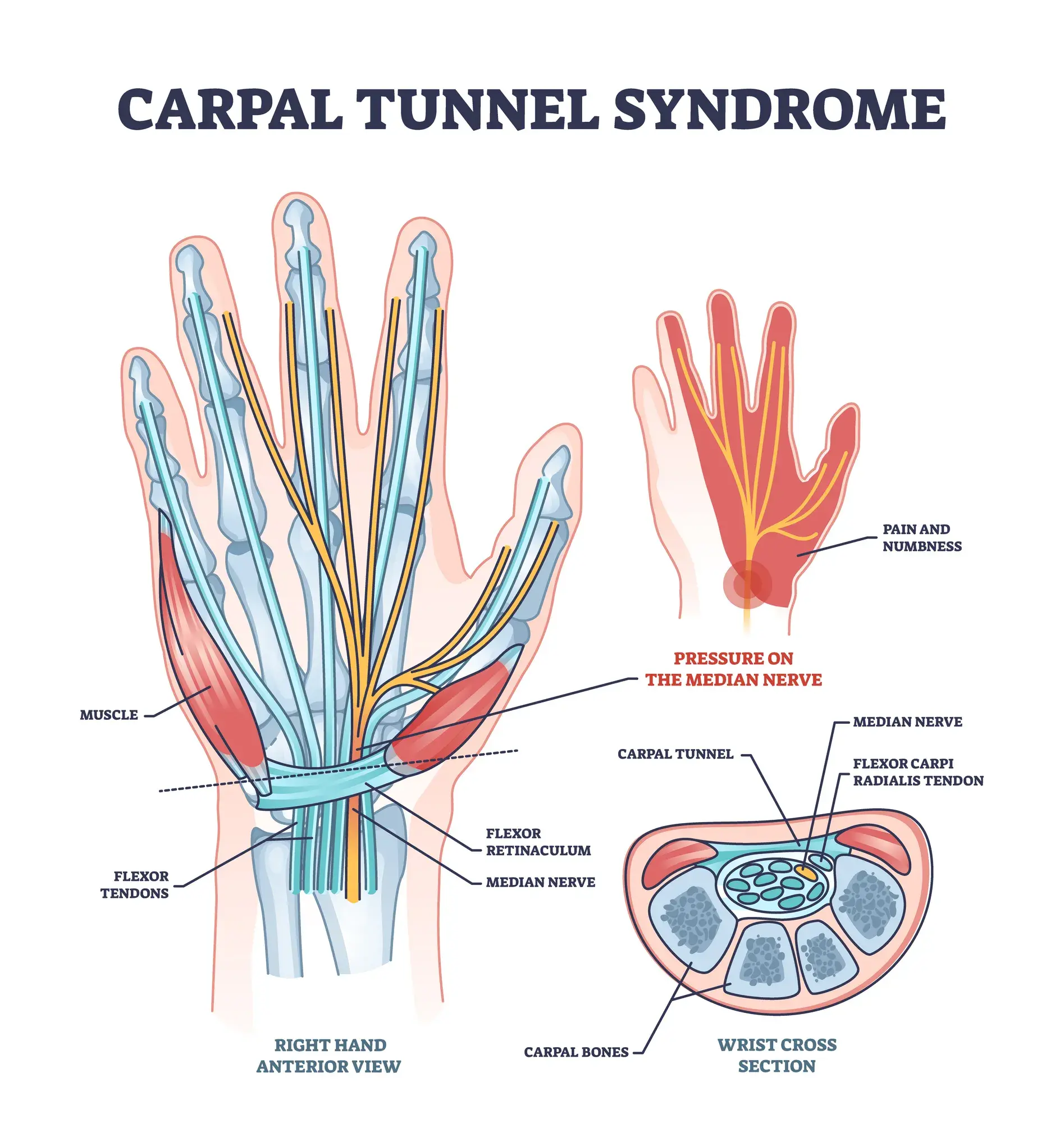
The causes of CTS vary, and this condition usually develops due to a combination of factors that increase pressure on the median nerve and tendons in the carpal tunnel. These risk factors include obesity, repetitive hand use, pregnancy, and conditions like diabetes or RA.
In particular, RA can increase the risk of CTS by causing the inflammation of the synovium (the lining of the joint) and the tenosynovium (the lining of the tendons). Inflammation leads to the build-up of fluids and swelling, which can narrow the carpal tunnel and cause CTS. It is estimated that up to a third of patients with RA will develop CTS.
Heart Problems
Heart problems, formally known as cardiovascular disease, refer to a range of conditions that affect the heart and blood vessels, like coronary artery disease, heart attack, heart failure, and stroke.
These conditions can stem from a myriad of factors like poor diet habits, high blood pressure, elevated cholesterol, smoking, genetics, diabetes, and a lack of physical activity. However, often, the universal cause of heart problems is systemic inflammation.
The symptoms of heart problems can vary significantly, depending on the condition that’s affecting you. Commonly, you may experience chest pain, shortness of breath, lightheadedness, fainting, and pain (especially throughout the chest and upper body). Since certain heart problems can be fatal, early detection and treatment are essential to prevent life-threatening complications.
RA can be a risk factor for cardiovascular disease. This is because the underlying chronic inflammation in RA can affect and damage the heart muscle, as well as critical blood vessels and surrounding areas.
Uncontrolled inflammation can also lead to the development of atherosclerosis, a condition that causes the arteries to harden and narrow, increasing the risk of heart disease. It is estimated that people with RA have a 50-70% higher risk of heart problems compared to the general population.
Lung Disease
Lung disease is a broad term that describes any disorder that involves dysfunction of the lungs or other parts of the respiratory system. Lung disease can cause anything from chronic conditions like asthma and chronic obstructive pulmonary disease (COPD) to cancers and acute infections such as pneumonia.
Common causes of lung disease include smoking, exposure to harmful pollutants and chemicals (e.g. asbestos), genetic factors, a compromised immune system, and even certain types of infections.
RA may also be a contributing factor in lung disease. This is due to the fact that the chronic inflammation occurring in the joints can spread to the lungs and cause scarring, which may lead to the development of a condition called rheumatoid lung disease.
This complication is present in nearly 5% of older patients with RA, and it can cause shortness of breath, persistent coughing, and chest pain, as well as fatigue, unexplained weight loss, and changes in voice tone.
Lymphoma
Lymphoma is a type of cancer that originates in the lymphatic system, the part of your immune system involved with maintaining fluid levels in the body and combating infections and diseases. While the root cause of lymphoma is still unknown, certain risk factors have been identified.
These include age (especially in adults over 55), a weakened immune system, exposure to certain chemicals, and even certain infections caused by viruses or bacteria. If left unaddressed, a lymphoma can cause life-threatening tumors in the lymph nodes.
Research has shown that people with RA have a two-fold increased risk of developing lymphoma. This is because uncontrolled high levels of inflammation can lead to cell damage, which is the root cause of lymphoma.
How Is RA Diagnosed?
There is no specific diagnostic test that can be used to prove you definitely have RA. What’s more, the early symptoms of RA overlap those of other conditions, which often leads to patients having to wait an average of nearly 17 months before initiating treatment.
Nonetheless, your doctor may use a wide range of examinations and laboratory tests to determine the source of your pain. If your doctor suspects that you have RA, they may refer you to a rheumatologist to confirm the diagnosis. Below, we’ll look at the most commonly used tests in more detail.
- Medical history
Since the symptoms of RA develop over time, it can be hard to confirm a diagnosis when your disease is in its early stages. However, your doctor may suspect that your symptoms are related to RA if you have a family history of RA or other autoimmune diseases.
A healthcare provider will also review influencing aspects, such as your general health, medications you take, and your symptoms.
- Physical examination
After reviewing your medical history, a doctor will carry out a physical examination. This exam isn’t painful, but it commonly involves the palpation of areas of the body that may be painful. A medical team will also look for signs of inflamed tendon sheaths (the lining of the tendons), tender joints, limited range of motion, and early deformity. If your symptoms are severe, they may also look for tendon tears and ruptures.
Since RA can develop across multiple joints in the body, it is important to tell your doctor about all the symptoms you are experiencing, even if they may seem unrelated to each other at first.
- Laboratory tests
Although it isn’t possible to diagnose RA using a single laboratory test, when analyzed together, the following examinations can be extremely helpful in making a diagnosis. These tests include:
Rheumatoid factor (RF): The RF test is a specific blood examination carried out to detect the presence of RF, a type of protein produced by your immune system. It is estimated that 60-80% of people with RA have RF.
Nonetheless, it is possible to have RA even if you test negative for RF (seronegative rheumatoid arthritis). Additionally, only 40% of those with early RA test positive for rheumatoid factor.
Anti-cyclic citrullinated peptide antibody (anti-CCP). The anti-CCP test is used to confirm the presence of RA after a rheumatoid factor test. It detects anti-CCP antibodies, a protein often present in people with RA. The anti-CCP test is more accurate than the RF test, and people who test positive are very likely to get RA.
Complete blood count (CBC). CBC is a type of blood test often used to examine components of the blood like red blood cells, white blood cells, and platelets. Detecting abnormalities in these areas can provide insight into inflammation or iron deficiency caused by low red blood cells (anemia), both common indicators of RA.
Erythrocyte sedimentation rate. The ESR or Sed rate is a commonly used blood test to measure the rate at which red blood cells settle at the bottom of a test tube in one hour. If the cells sink faster than normal, this indicates higher-than-normal levels of inflammation. This test can also be used to monitor how inflammation levels change over time.
C-reactive protein. CRP is a substance produced by the liver in response to inflammation. Elevated levels of CRP can indicate high inflammation, which is typical in RA. CRP levels are also used to assess the extent of inflammation in the body and to monitor the effectiveness of RA treatments.
- Imaging tests
Imaging tests can be used to obtain a clear picture of the inner aspect of your joints. These tests allow your doctor to determine the presence of inflammation, abnormalities, and, in the case of an RA diagnosis, the extent of the damage. Different tests can be used to examine different types of soft and hard tissues. These include:
X-ray. By emitting a concentrated beam of radiation toward the joints in question, an X-ray can provide detailed images of dense structures like bone. These images will allow your doctor to spot any physical alterations or damage in your joints, such as bone erosions or narrowing of the joint space. These symptoms are not present in the early stages of RA; however, your doctor may still use X-rays to rule out other conditions.
Computed tomography scan (CT Scan). A CT scan works like an advanced X-ray machine. It creates multiple images from different angles around the body and produces a detailed cross-sectional view. CT scans can reveal the details of bone damage that might not be clear in standard X-rays.
Magnetic resonance imaging (MRI). MRI captures high-resolution images of your joints using strong magnetic fields and radio waves. It reveals the presence of inflammation and early joint damage and tracks disease progression – something that may not be visible through other scans.
Positron emission tomography (PET scan). A PET scan works by detecting radioactive material injected into your body. This material, known as a radiotracer, releases positrons, which interact with electrons in your body. This interaction causes the production of gamma rays, which are picked up by PET scanners. These advanced imaging tools can examine how tissues and organs are functioning, and they can precisely determine the extent and location of inflammation.
Dual-energy X-ray absorptiometry (DEXA). DEXA works by directing two X-ray beams of varying energies toward the patient’s bones. By analyzing the different rates of absorption for these X-rays, doctors can obtain precise information about bone density and other abnormal changes.
These tests, alongside ultrasound scans and more specific laboratory tests, can be used as stand-alone diagnostic tools or in combination with other methods to determine the presence of RA.
Common Treatment Options For RA
As mentioned above, there is no permanent cure for RA. However, several treatment plans can help you manage your symptoms and even modify the disease. The most common goals for treatment for RA include:
- Easing symptoms
- Putting the disease into remission by stopping inflammation or reducing it to the lowest possible level
- Preventing permanent damage to joints and surrounding organs
- Preventing long-term complications
To achieve these goals, your doctor may use medications, conservative treatments, and surgical interventions to reduce inflammation as quickly as possible, monitor the levels of inflammation, and work toward low or no symptoms.
You may also be recommended a range of lifestyle modifications that can help you lower inflammation and manage your symptoms. These include changing your diet, losing excess weight, making movement part of your daily routine, and ensuring a focus on quality sleep and stress management.
In the sections below, we’ll explore the traditional treatments prescribed for RA, as well as their benefits and limitations.
Medication
Medications are often the first port of call for patients with RA and healthcare providers alike. There are several types of medications that may help with this condition, and they can be subdivided into two categories:
- Medications that don’t modify the disease but relieve its symptoms. These include painkillers, non-steroidal anti-inflammatory drugs (NSAIDs), and corticosteroids
- Medications that modify the course of the disease. These include disease-modifying anti-rheumatic drugs (DMARDs), which can be biologic or nonbiologic and are managed by a rheumatologist.
These drugs are often used in combination, to tackle multiple aspects of the disease. What’s more, when complications of RA occur, these comorbidities may also need to be addressed. As a result, many patients follow a complex medication regimen that involves more than one drug. Below, we’ll look in more detail at treatment options available today:
- Painkillers
Painkillers are often available as over-the-counter alternatives that can help you manage the symptoms of RA in an accessible and affordable way. While these drugs don’t modify the course of the disease, they can be used to ease flare-ups.
- Corticosteroids
These are the manufactured versions of a hormone that is naturally produced by the body, cortisol. They can be administered in the form of tablets or directly injected into the joint. They can be used as a short-term alternative to relieve pain and inflammation flare-ups, or while you are waiting for DMARD medications to start working.
Taking these medications chronically can have serious side effects, including weight gain, skin thinning, joint damage, osteoporosis, and a serious condition known as adrenal gland insufficiency.
- Non-steroidal anti-inflammatory drugs (NSAIDs)
NSAIDs can reduce pain and inflammation by blocking the COX enzyme, which is responsible for the production of prostaglandins. Prostaglandins are a hormone-like substance responsible for regulating body functions such as inflammation and pain perception. NSAIDs are usually available as over-the-counter alternatives, and they include drugs such as ibuprofen and aspirin.
- Disease-modifying anti-rheumatic drugs (DMARDs)
DMARDs work by inhibiting an overactive immune system, thus reducing the inflammation associated with an abnormal immune response. They can be delivered via subcutaneous injections or intravenously.
When accurately managed and monitored by a rheumatologist, these drugs can help ease inflammation and prevent the complications of RA, including joint damage. Not all types of DMARDs work equally well for all patients.
There are three main types of DMARDs:
Nonbiologic DMARDs: These are conventional drugs that work by suppressing the entire immune system, and they include methotrexate and sulfasalazine. It can take months for these DMARDs to start working and, in the meantime, your doctor may prescribe pain-killing medications like prednisone.
Biologic DMARDs: These are a newer class of drugs that work by targeting specific parts of the immune system or certain cell types responsible for inflammation. While these are more expensive, they are faster-acting, and you’ll be able to see if these drugs work for you within two to six weeks.
Janus kinase (JAK) inhibitors. These are a new class of drugs that works by inhibiting the messaging pathway that leads to the production of inflammatory cells known as cytokines. This calms down the immune system and helps ease the symptoms of RA.
It is important to keep in mind that DMARDs aren’t free of side effects, which include liver damage, nausea, high blood pressure, and, due to the fact that they suppress the immune system, an increased risk of serious infection.
Heat And Cold
One of the most popular at-home care strategies for rheumatoid arthritis relief is the application of an ice pack or hot compress. These work in two different ways, and you may find that one works better than the other for your specific needs.
Ice works by constricting blood vessels, which can reduce inflammation and swelling. This can temporarily ease joint pain and stiffness, thus boosting your joints’ range of motion and reducing disability. On the other hand, heat increases the circulation of blood and oxygen in and around the damaged joints. It can also help to relax the muscles, ease pressure on the nerves, and induce a generalized sense of well-being, which can help you better manage RA pain.
This technique does not cure the disease itself, however. It’s merely an easy option for symptom management during particularly unbearable flare-ups. And, in any case, hot compresses and ice packs are best used in conjunction with other prescribed treatments, such as medication or physical therapy. Additionally, while they are generally safe, these at-home care methods can have side effects such as skin irritation and discomfort.
Joint Immobilization
Joint immobilization is a treatment approach for RA that works by restricting movement. This can prevent further damage to an already injured joint and can relieve undue pressure during physical activity and sports.
Common immobilization techniques include wearing a brace or splint, which stabilizes the joint and minimizes stress on the affected area. While this treatment option is generally safe, it is important to follow the instructions of your rheumatologist. Overuse of joint immobilization can lead to stiffness, muscle weakness, and loss of muscle mass (atrophy), which can further affect your musculoskeletal health over time.
Massage
Massage therapy may be used as a conservative treatment to alleviate the symptoms of RA. It works by reducing muscle tension and easing the pressure on nerves and joints. In turn, you may find that massages can improve your mobility and reduce pain. Studies have also shown that certain massage techniques, such as Swedish massages, may help relieve pain and reduce the need for pain medications in people with RA.
Nonetheless, this treatment option is not equally effective for everyone, and some may even experience temporary discomfort following each session. If you are looking to explore massage therapy as an option to manage your RA symptoms, be sure to work with a massage therapist who specializes in RA treatments.
Acupuncture
Acupuncture is becoming an increasingly popular alternative method for managing the symptoms of RA. The original belief at the center of this healing methodology is its power to unblock Qi, the supposed life energy flowing within each person.
Nonetheless, research attributes the beneficial effects of acupuncture to this therapy’s ability to trigger the release of endorphins and other neurotransmitters responsible for pain modulation and feelings of well-being. Studies also show that acupuncture can effectively ease the symptoms of RA, improve quality of life, and boost function without causing side effects. This is thanks to the anti-inflammatory, antioxidative, and immuno-regulatory effects of acupuncture.
Acupuncture does not work equally well for everyone and may not be recommended for those with bleeding disorders or taking blood thinning medications.
Surgery
If your RA isn’t responding well to conservative treatments or it has caused permanent damage to the joints and disability, your doctor may recommend surgery. Different types of orthopedic surgical interventions may help reduce the complications of RA. These include:
- Synovectomy. This surgery involves removing the lining of a synovial joint that has been affected by RA. While this surgery can ease pain, it is only indicated in the early stages of RA or if the inflammation is only affecting the synovium. It does not prevent the disease from progressing or affecting other joint components.
- Tendon repairs. If you have suffered tendon tears or ruptures, this surgical intervention can help repair the tendon through grafts. Tendon surgeries can also be performed to strengthen the tendons and prevent ruptures, release tight tendon tunnels, and remove inflamed tissue.
- Joint rebalancing. Joint rebalancing can address deformities and contractures (which occur when the joint’s tissues become stiff or shortened), thus improving joint function and reducing pain.
- Joint replacement surgery. This surgery, known as arthroplasty, involves replacing damaged parts of the joint with artificial components made of plastic or metal to restore function.
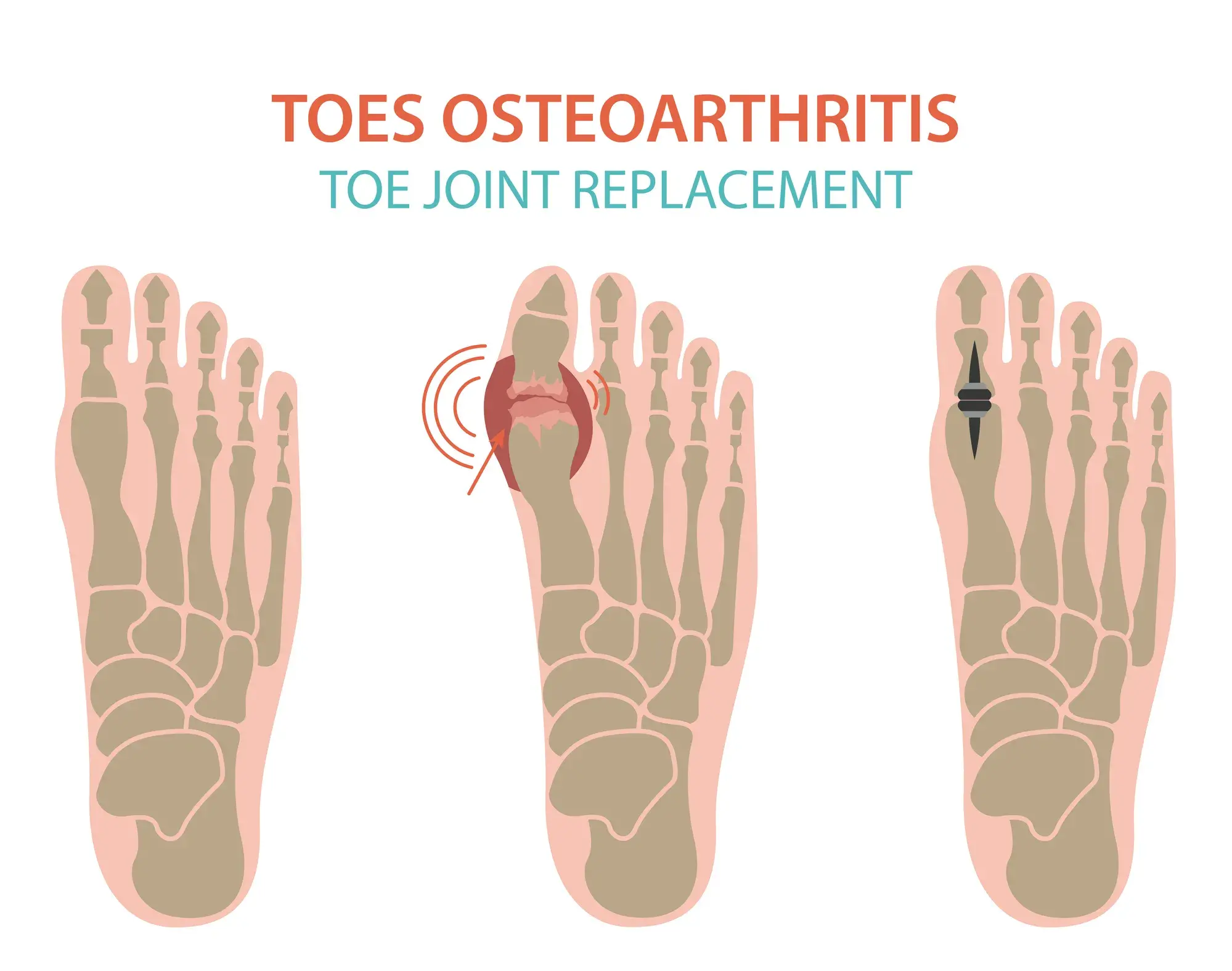
- Joint fusion. This surgical intervention fuses together two bones to make one bone. During this surgery, the remaining damaged cartilage is removed from each side of the joint and the ends of the bones are reshaped to fit together. While joint fusion removes pain, it also eliminates the joint’s ability to move. Because of this, this type of surgery is preferred over arthroplasty only in the case of small joints that don’t compromise mobility, such as those in the hands and fingers.
Regardless of the type of surgery, there are risks that cannot be overlooked. Besides the lengthy and painful rehabilitation periods involved with invasive interventions, surgery can carry severe risks like infections, adverse reactions to anesthesia, and damage to nerves and other components of the joint. Additionally, surgical interventions may not be able to entirely stop the pain or prevent RA from progressing. If you are considering surgery, you should work with an orthopedic specialist or rheumatologist who can help you better understand the benefits and drawbacks of this choice.
Our Approach To Treating Rheumatoid Arthritis
If you have been diagnosed with rheumatoid arthritis, the chances are that you are facing two equally undesirable prospects: living a life reliant on medications or undergoing painful surgeries. Fortunately, thanks to today’s advances in research, new treatment options exist that don’t involve invasive interventions or drugs.
RELATYV Mobile Pain Management works by addressing the uncontrolled systemic inflammation that’s aggravating your symptoms – and increasing your risk of developing chronic inflammatory conditions like cardiovascular disease and lung problems. This innovative whole-person approach does more than simply ease the pain: it combats systemic inflammation, supports the regeneration of damaged tissues, and lays the foundations of long-term musculoskeletal health.
Below, we’ll explore the three non-drug, non-invasive, and non-chiropractic therapies at the core of Neurofunctional Pain Management.
Electroanalgesia
Electroanalgesia is a pain management technique that uses high-pulse electrical current to ease pain, boost blood circulation, improve mobility, and induce...
IV Therapy
IV nutritional therapy, or intravenous therapy, involves administering vital nutrients directly to the bloodstream through an IV. This type of treatment bypasses the digestive system, allowing for maximum absorption and utilization of nutrients by the...
Lifestyle Counseling
Lifestyle counseling is an approach to managing chronic pain that involves identifying, assessing, and modifying lifestyle factors contributing to an individual's pain. For example, lifestyle factors such as nutrition, physical activity, stress, sleep quality...
Embrace A Healthier You – Manage Your RA Symptoms Effectively
Receiving a diagnosis of RA can truly be life-changing. The pain and dysfunction can affect your daily life, and the lack of available cures can make this burden unbearable. Fortunately, medications and surgery are no longer the only options available to effectively manage your symptoms.
With the approach, RELATYV Mobile Pain Management, you can take a concrete step toward optimal health and magnify your quality of life.
Get started today and take action against rheumatoid arthritis!



