Metabolic dysfunction is a complex disorder that affects one in three adults in the US and dramatically increases a person’s risk to suffer from heart disease, stroke, and diabetes.
Often caused by risk factors such as inactivity, obesity, and high blood pressure, this condition can lead to a cascade of symptoms, including systemic fatigue and inflammation.
Despite how widespread metabolic dysfunction is, diagnosing it remains a clinical challenge. In turn, most patients are stuck with pharmacological treatments that are ineffective at best and dangerous at worst.
Fortunately, you can easily address metabolic dysfunction and prevent the life-limiting complications it causes by modifying some key lifestyle factors. Let’s look at how the innovative whole-person approach by RELATYV can help you kickstart your journey toward regaining your health – without medications, surgery, or chiropractic therapies.
What is Metabolic Dysfunction?
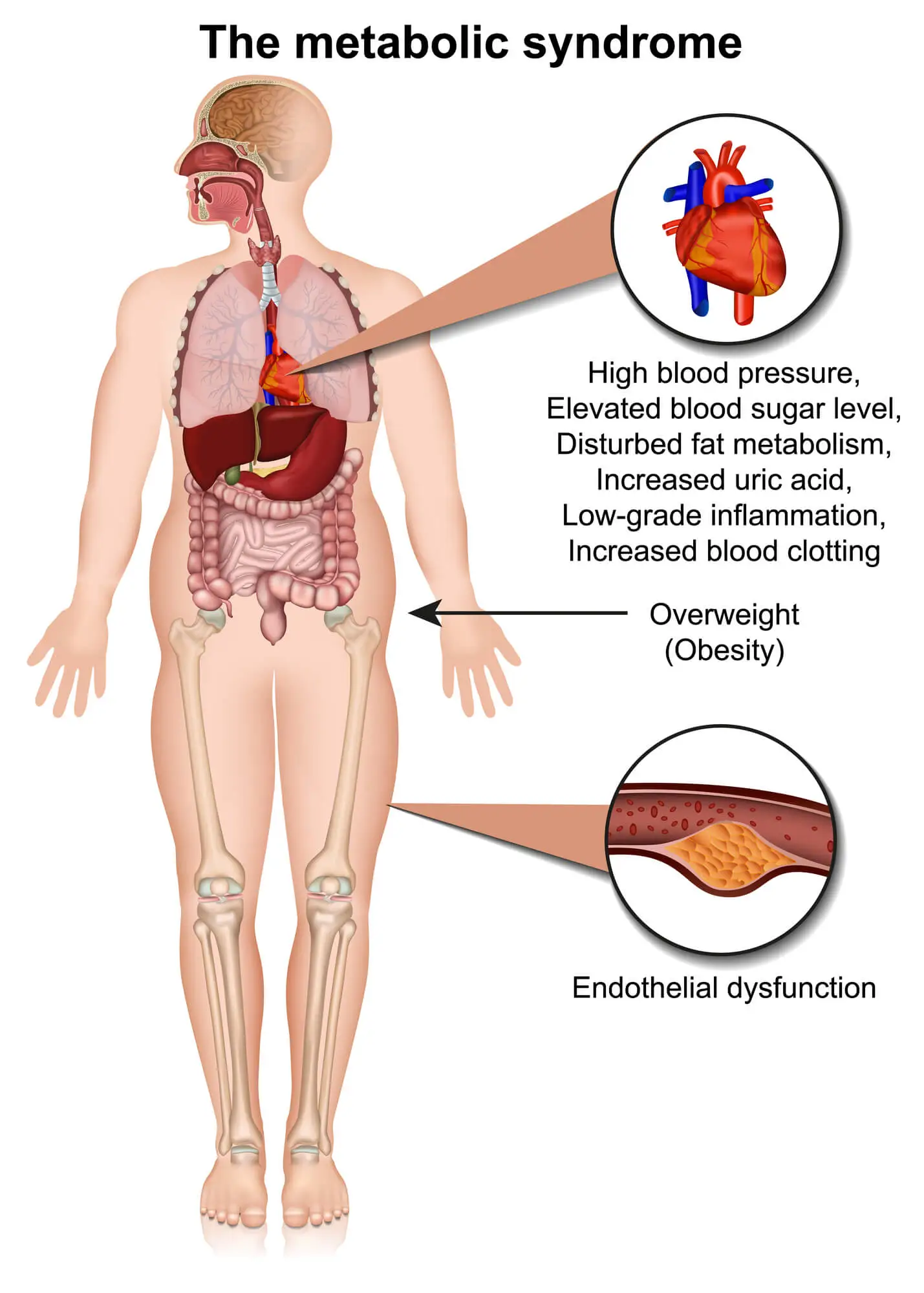
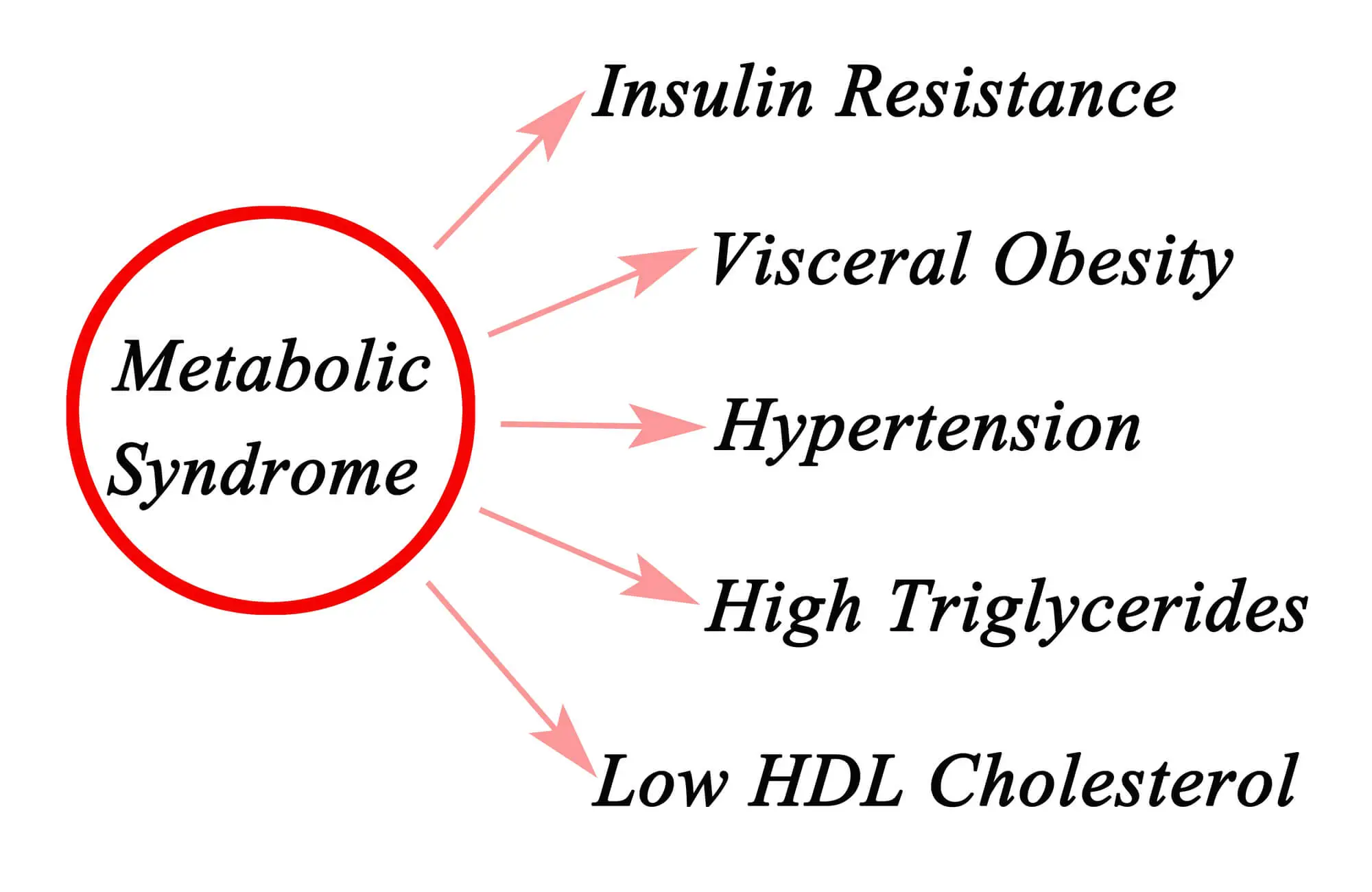
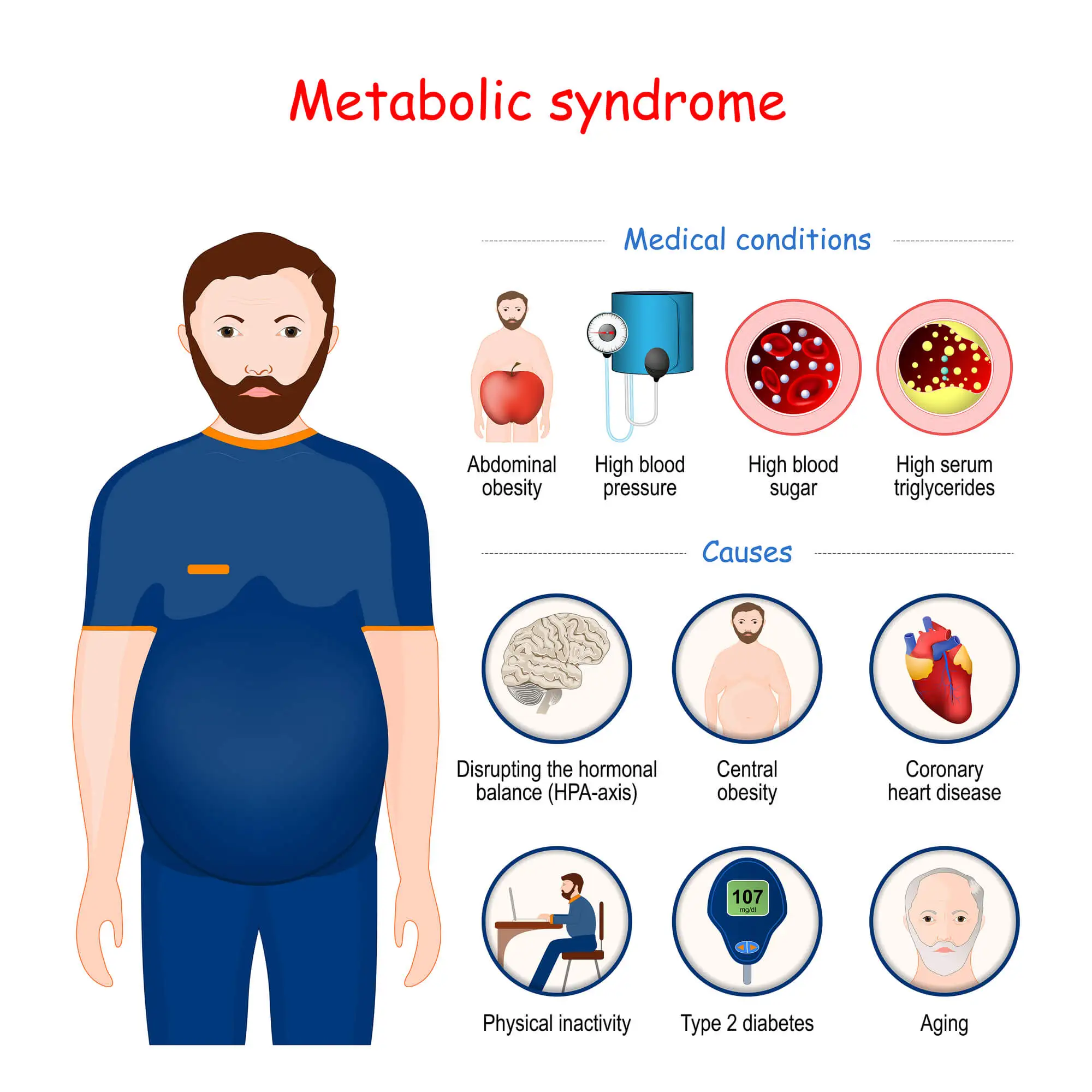
Metabolic dysfunction is a term used to describe a cluster (or group) of conditions. When these conditions occur at the same time, they drastically increase your risk of suffering from diabetes, stroke, and heart failure. These conditions include high blood pressure, high blood sugar levels, high blood triglycerides, and a larger waistline.
To better understand what metabolic dysfunction is and how it develops, it is crucial to cover the basics of the body’s metabolic processes.
Metabolic Processes and Metabolic Dysfunction
Metabolism refers to all of those processes and chemical reactions used by the body to break down the nutrients contained in the food you eat to produce energy. During this process, carbohydrates, protein, and fats are transformed into acids and sugars – the body’s fuel – which are either stored or used for energy. Several components of the body contribute to keeping the metabolic process healthy, including hormones, cells, and organs.
If abnormal chemical reactions or diseased organs disrupt this complex process, you may develop metabolic dysfunction. Depending on what aspects of the metabolism are affected, you may suffer from one or more types of metabolic disorders, such as the following:
- The body is unable to break down some nutrients (such as carbohydrates or proteins) due to the lack of certain chemicals (enzymes) that play a role in the metabolic process.
- The part of the cells in charge of transforming sugar into energy – mitochondria – is inhibited. This prevents the cell from obtaining the energy needed to carry out biochemical processes and causes a build-up of sugar in the blood.
- One or more of the organs involved with the metabolic process is not working properly.
How Metabolic Dysfunction Manifests Itself
According to a 2017 study, the prevalence of metabolic disorders has increased by 35% between the 1980s – when this disease was first categorized – and 2012. The rates of metabolic dysfunctions are also increasing alongside the prevalence of obesity.
People with metabolic disorders experience a range of symptoms, including high blood pressure, high blood glucose, and a high level of triglycerides in the blood. These conditions increase the risk of cardiovascular disease, diabetes, and heart failure.
But while metabolic imbalance is widespread and life-threatening, diagnosing remains a clinical challenge. This is because, besides an abnormal accumulation of fat around the waistline, the symptoms of this condition don’t manifest themselves easily. Nonetheless, obtaining an early diagnosis is essential to avoid the most severe complications of metabolic dysfunction through treatment and positive lifestyle changes.
Two Types Of Metabolic Dysfunction
While there are several types of metabolic disorders, they can be categorized based on what part of the metabolic process is affected or disrupted. In particular, disruptions can occur during one of two processes: catabolism or anabolism.
Catabolism
Catabolism refers to the metabolic process the body uses to produce energy. During the catabolic phase, larger molecules – such as the ones found in food’s fat, protein, and carbohydrates – are broken down into smaller compounds. For example, carbohydrates are transformed into glucose.
Disorders that disrupt this process prevent the body from accessing essential energy sources, such as sugar and acids.
Anabolism
During the anabolic phase, the body uses the energy obtained from food to fuel essential bodily functions, like building new cells and maintaining tissues such as bones and muscles. The energy that is not immediately used is then stored in the liver and muscles for later use.
Metabolic disorders that disrupt this process impact the body’s ability to use and store energy.
Symptoms of Metabolic Dysfunction
Metabolic dysfunction is likely to develop if you have three or more of the following risk factors:
- Abdominal obesity: This is the excessive accumulation of fat around the waistline, a condition that gives your body an “apple shape”. Compared to the build-up of fat in other areas of the body, abdominal obesity represents a major risk factor for heart disease.
- Hypertension: Having high blood pressure for prolonged periods can cause damage to the blood vessels and heart, making it a predictive factor for heart disease.
- Hyperglycaemia: High blood sugar levels increase the risk of blood clots and damage to the blood vessels.
- High levels of blood triglycerides and LDL (“bad”) cholesterol: These are types of fats that circulate in the blood responsible for storing and using energy. Too much of these fats in the blood can lead to heart disease.
- Low levels of HDL cholesterol: HDL – or “good” – cholesterol is a compound that absorbs the “bad” cholesterol in excess and carries it back to the liver for expulsion. Low levels of HDL cholesterol translate into high levels of LDL cholesterol, which can clog the blood vessels and cause heart failure or stroke.
So, for many patients, the only telltale sign that they may have metabolic imbalance is a larger waistline. That is until comprehensive blood tests are carried out.
However, you may also experience other symptoms directly related to the conditions above. Let’s look at these below.
Nausea, Tiredness, And Weakness
Metabolic disorders prevent your body from absorbing essential nutrients or transforming molecules into energy, which can cause you to feel tired or experience gastrointestinal problems (i.e.: nausea).
Some rare metabolic conditions such as glycogen storage disease (GSD) may also inhibit your body’s ability to store glycogen (a type of blood sugar). This leads to muscle weakness and chronic fatigue.
Unexpected Weight Gain Or Loss
If your body is unable to process nutrients as it should, you may experience unexpected weight gain. However, metabolic dysfunction may also lead to reduced appetite, which can cause involuntary weight loss.
Your Body Mass Index and weight history are also closely related to your risk of developing metabolic disorders.
Changes In Skin Color
If you have diabetes – the most common metabolic disorder – you may experience a range of symptoms. Firstly, uncontrolled levels of blood glucose can clog and narrow the blood vessels, leading to complications such as blurred vision. Additionally, as the excess glucose in the blood is expelled through urination, you may have an increased need to urinate. This can make you dehydrated and increase sensations of thirst.
Lastly, diabetes can cause changes in the color and texture of your skin. This occurs when the ineffective insulin in excess that builds up within the blood vessels increases the concentration of melatonin (pigment) on the skin. In turn, you may notice darker patches on your skin, usually at the front of your legs or shins.
Stomach Pain
Metabolic dysfunction may lead to gastrointestinal problems, such as nausea and vomiting. Some disorders – such as hypertriglyceridemia (high levels of triglycerides) – can also manifest themselves as stomach or abdominal pain.
According to a 2016 study, metabolic dysfunction may also cause pain in other areas of the body (such as the knees) by aggravating the effects of inflammatory conditions like osteoarthritis.
Cognitive Impairment
Cognitive impairment describes any decline in cognitive abilities, such as memory, language, problem-solving, and attention. Such impairments can be a sign of more serious conditions, such as dementia or Alzheimer's disease, but they can also be the result of...
Tiredness, Nausea, and Weakness
If you are struggling with chronic tiredness, weakness, and nausea, you may be battling limitations in all aspects of your everyday life - from reduced productivity at work to pain, discomfort, and low energy levels. And the situation may be made worse by the...
Sudden Weight Gain Or Weight Loss
Unexpected weight change can have serious implications for your health. However, there are steps you can take to manage this change and reduce the risk of associated health conditions. It's essential to speak to a doctor if you experience sudden weight...
Excess Gas In The Stomach
Are you experiencing stomach bloating or excess gas? Discover the causes, symptoms, and effective remedies to manage gas pain with Neuragenex...
Digestive Issues
Digestive upset is a common issue we can all experience from time to time. However, if your digestive issues are an ongoing struggle and become more than just a minor inconvenience, perhaps they’re a sign of an underlying condition....
Causes of Metabolic Dysfunction
The reasons why a person develops metabolic imbalances are not always clear. However, in most cases, a role is played by genetic factors, autoimmune diseases, organ malfunction, or dysfunction in processes at a cellular level.
Understanding what may be increasing your risk of developing metabolic dysfunction is critical for early detection. Let’s look at the most common causes of this condition below.
Genetics
Genetic factors – which are passed down through families – play a significant role in a person’s risk of developing metabolic dysfunction. For example, genetic mutations may cause the body to produce too much or too little of certain enzymes that play a role in breaking down molecules such as fats.
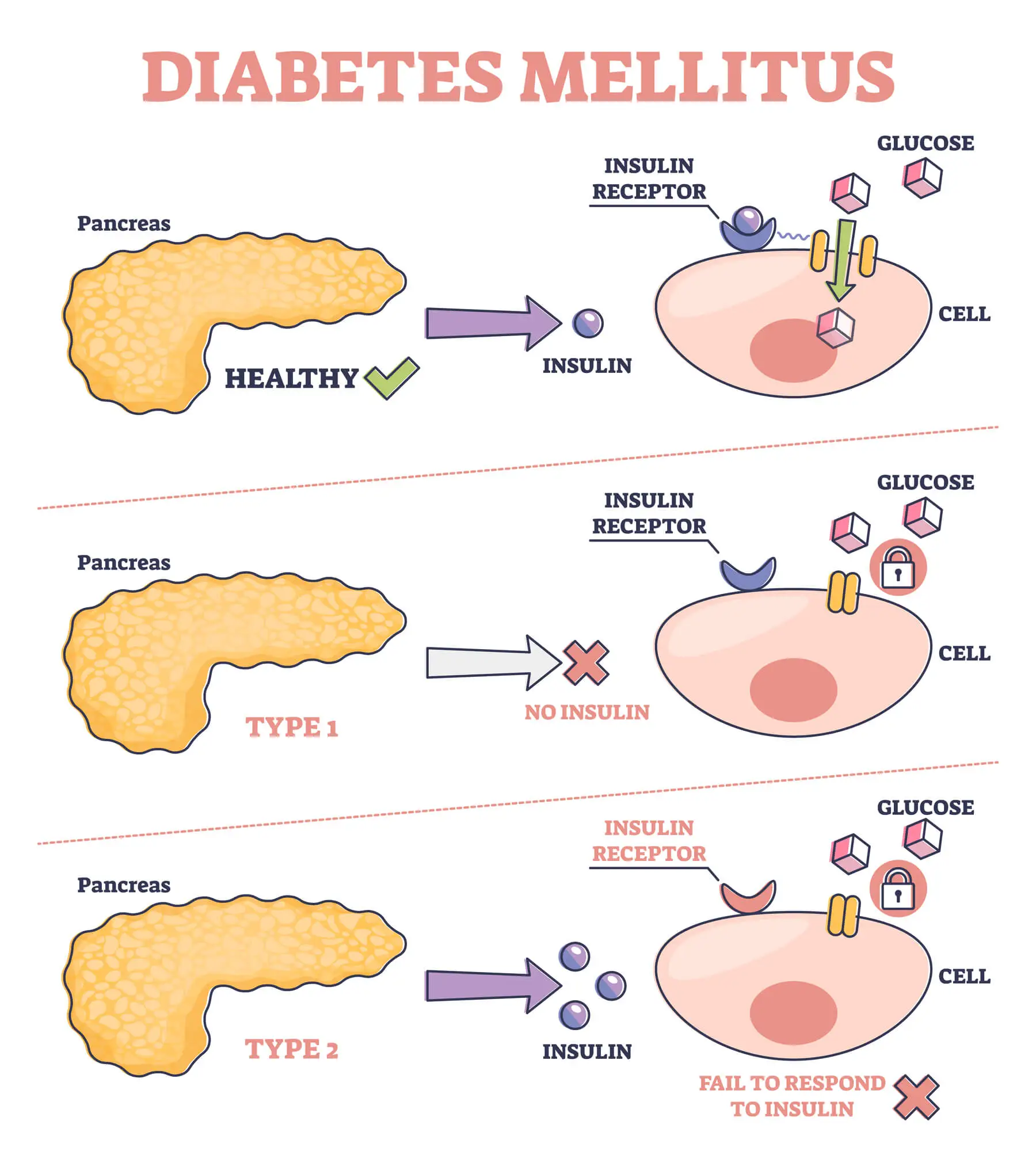
Metabolic disorders may also be caused by autoimmune diseases, in which the immune system mistakenly attacks the body’s tissues. For instance, in people with Type 1 diabetes, the cells in the pancreas responsible for creating insulin are destroyed by the immune system. Without insulin, blood sugar is unable to enter the cells, which translates into an abnormal build-up of glucose in the blood.
Organ Dysfunction
Metabolic imbalances may develop if the organs that contribute to the metabolism fail to function properly. For example, if the liver or pancreas doesn’t work as they should, they may not be able to produce the enzymes necessary to break down food or expel waste.
An overactive or underactive thyroid may also contribute to metabolic imbalances by providing too much or too little of certain hormones involved in maintaining the rate of metabolism.
Mitochondrial Dysfunction
Metabolic imbalance may occur at a cellular level. This is the case of metabolic disorders caused by mitochondrial dysfunction.
The mitochondria is the part of the cell responsible for producing energy from blood sugar. The cells’ mitochondria can be affected by mutations of the DNA as well as genetic factors and environmental triggers. When this happens, the cells are unable to create the necessary energy to fuel bodily processes such as the creation of new tissue. This results in muscle shrinking, weakness, and diabetes.
Common Risk Factors
A person’s weight is one of the most predictive risk factors for metabolic disorders. This is because, in obese and overweight people, extra fat cells – especially when they accumulate around the waistline – can increase the levels of “bad” LDL cholesterol, blood pressure, and blood triglycerides, while lowering the levels of “good” HDL cholesterol.
Excessive weight is also becoming a more prevalent risk factor due to the fact that the rates of overweight, obesity and severe obesity are rising.
Other critical risk factors for metabolic imbalance include the following:
- Age: Metabolic processes and speed change as we age, which can cause weight gain and increased risk of metabolic imbalances.
- Ethnicity: Some genetic mutations are more likely to be passed down through families within certain racial or ethnic groups. For example, maple syrup urine disease is more common among Mennonite communities, and sickle cell anemia among African Americans.
- Environment: Having a low socioeconomic status may be related to an increased risk of obesity, overweight, and a sedentary lifestyle, which are major risk factors for metabolic disorders.
- A history of overweight and obesity: Being obese during pregnancy may increase a newborn’s risk of suffering from metabolic disorders. Additionally, children who rapidly gain weight after birth may be more likely to develop metabolic syndrome later in life.
- A history of diabetes: If close relatives suffer from Type 1 (hereditary) diabetes, you may be at greater risk of suffering from the same metabolic disorder.
- Type 2 diabetes: If you have Type 2 diabetes, your body may be unable to transform blood sugar into energy. This makes other components of metabolic dysfunction – such as high blood sugar and high blood pressure – more likely.
- Low cholesterol: Low levels of “good” HDL cholesterol may lead to an accumulation of “plaques” of bad cholesterol in the blood vessels and arteries. This increases your risk of stroke and heart attack.
- High blood pressure: Hypertension is related to disruptions in the process that allows the body to obtain energy from nutrients at a cellular level. As such, it can be considered a metabolic disorder in itself. It is also a risk factor for heart disease, stroke, and diabetes.
- High triglycerides: If you have high levels of triglycerides, you may be at risk of complications such as the hardening of arteries, stroke, and heart disease.
Besides genes and autoimmune disease, most of the risk factors above derive from lifestyle elements such as being inactive, eating an unhealthy diet, smoking, drinking alcohol, and having sleep problems. These factors can be addressed through adequate treatment – let’s look at this in more detail below.
Diagnosing Metabolic Dysfunction
As seen above, diagnosing metabolic dysfunction can be challenging, especially as a larger waistline is often the only visible symptom of this condition. However, if you have noticed unexpected weight gain or loss, or your family history puts you at risk of developing metabolic disorders, your doctor may prescribe a series of diagnostic tests.
- A review of your family and medical history to identify genetic causes or inherited metabolic diseases
- A physical exam that includes a measurement of your waist and Body Mass Index
- A review of your lifestyle, such as units of alcohol, frequency of exercise, and dietary choices.
- Blood tests to check for abnormal glucose, cholesterol, and triglyceride levels.
- Blood pressure tests
Your condition may be classified as metabolic dysfunction if you have three or more of the following:
- A waist circumference larger than 40 inches for men and 35 inches for women
- Blood pressure consistently higher than 130/85 mmHg (millimeters of mercury)
- Fasting blood sugar levels higher than 100–125 mg/dL (milligrams per deciliter)
- “Good” HDL cholesterol levels lower than 50 mg/dL for women and 40 mg/dL for men
- Blood triglyceride levels consistently higher than 150 mg/dL
Treatment Options for Metabolic Dysfunction
When it comes to treating metabolic dysfunction, doctors tend to prescribe medicines that aim to control one or more of the conditions that, together, increase the risk of metabolic dysfunction.
Given that these therapies don’t cure the disease, people with metabolic dysfunction often require lifelong medications. This is especially true when drugs are used to address chronic conditions like diabetes.

Some of the most common treatment options prescribed for metabolic dysfunction today include:
- Insulin shots to manage blood sugar levels and diabetes
- Insulin sensitizers
- Medicines to lower your blood pressure, such as ACE inhibitors and diuretics
- Medications to lower blood triglyceride and “bad” cholesterol
- Medications to increase the levels of “good” HDL cholesterol
- Weight loss medicines to address overweight and diabetes
- Weight loss surgery that reduces the size of your stomach
These therapies may help you manage the complications of metabolic disorders in the short term, but they come with severe side effects such as digestive problems, liver damage, heart failure, anemia, and, in the case of surgery, damage to the stomach and intestines.
Does Medication-Only Help?
Medications for metabolic imbalance only treat the sub-conditions of this disorder, such as high blood pressure or high blood sugar levels. The aim of these therapies is often to reduce the risk of complications such as heart failure, stroke, or cardiovascular disease.
However, they don’t cure or modify metabolic dysfunction. Even worse, they can expose patients to severe side effects and cause them to live a life reliant on medications or surgery.
Fortunately, studies have shown that there is a different approach that can help you manage the symptoms of metabolic disorders without leading to complications: lifestyle and risk factor modification.
When introduced following early detection and diagnosis, heart-healthy lifestyle changes can help you re-establish the proper functioning of your metabolism and reduce the risks of metabolic syndrome.
A New Way Of Managing Metabolic Dysfunction
Whether you have just been diagnosed with metabolic dysfunction, are at risk of this disease because of a family history of diabetes, or are looking to better manage your condition, taking medications daily is no longer the only treatment option available.
Studies have proven the role of intensive lifestyle changes – especially regarding diet and exercise – to prevent the progression of metabolic disorders, prevent complications such as diabetes, and reverse metabolic dysfunction.
Here’s where Neurofunctional Pain Management (NFPM) comes in. This whole-person and science-backed approach provides a new way of managing metabolic imbalance without medications or surgery.
Following a complete examination and comprehensive blood tests, our specialists will provide you with Lifestyle Counseling services and IV therapies that aim to boost your overall health and address the risk factors that may be disrupting your metabolism.
Some of the approaches used include:
- Diet and nutrition guidance: A drastic change in your dietary regime can help reduce high blood pressure, boost nutrition, and ease inflammation.
- Weight loss coaching: Reducing your waistline and reversing a high Body Mass Index through diet and exercise can help you minimize your risk of suffering from cardiovascular and metabolic disorders.
- Positive lifestyle changes: A lifestyle counselor will help you quit smoking, reduce the consumption of alcohol, manage stress, and improve your sleep quality, thus addressing several of the main risk factors for metabolic dysfunction.
- IV therapies: Custom IV therapies provide long-lasting hydration, reduce inflammation, and correct any nutritional deficiencies that may arise as a consequence of metabolic dysfunction.
When coupled with electroanalgesia, RELATYV’s whole-person approach can help you free yourself of medications and the fear of having to undergo surgery.
Electroanalgesia
Electroanalgesia is a pain management technique that uses high-pulse electrical current to ease pain, boost blood circulation, improve mobility, and induce...
IV Therapy
IV nutritional therapy, or intravenous therapy, involves administering vital nutrients directly to the bloodstream through an IV. This type of treatment bypasses the digestive system, allowing for maximum absorption and utilization of nutrients by the...
Lifestyle Counseling
Lifestyle counseling is an approach to managing chronic pain that involves identifying, assessing, and modifying lifestyle factors contributing to an individual's pain. For example, lifestyle factors such as nutrition, physical activity, stress, sleep quality...
How Living With Metabolic Dysfunction Feels Like
The symptoms of metabolic dysfunction can develop over time. But, if left unaddressed, this condition can significantly increase the risk of developing cardiovascular diseases and diabetes. High blood pressure, high “bad” cholesterol, and high blood sugar levels can also lead to conditions such as plaque buildup (atherosclerosis), blood clots, coronary heart disease, heart failure, erectile dysfunction, stroke, organ damage, and chronic inflammation.
Fortunately, it is possible to manage metabolic dysfunction and reverse some of the conditions it causes by maintaining a healthy weight, exercising regularly, quitting smoking and consuming alcohol, and eating a diet rich in vegetables, fruit, legumes, and fiber.
Partnering with us can make it easier to live with this condition until its symptoms and complications are reversed.
Take The Next Step Toward Managing Your Condition
Although positive and heart-healthy lifestyle changes should be the first line of treatment for metabolic dysfunction, many patients see their lives tied to taking medications daily to address high blood pressure or glucose levels.
Our mission is to use a whole-person, science-backed approach to become the first thought and the first step in managing and treating metabolic dysfunction. A tailored treatment protocol based on your unique needs can help you restore your health and magnify your quality of life without medications or surgery.
Are you dealing with metabolic dysfunction? Stop suffering from the symptoms related to this condition.