Chronic headaches plague over half of the global population, but no two types of headaches have the same impact on a person’s life. Among these are cluster headaches, some of the most painful head conditions known today.
Also known as trigeminal autonomic cephalgia, cluster headaches only affect around 0.1% of the population. While rare, this condition can be excruciating and life-limiting.
Patients battling cluster headaches are often tied to taking pain medications and corticosteroids regularly or have to resort to occipital nerve injections to prevent or deal with acute attacks.
A lot is yet to be understood about this condition, but we now know that there are alternative treatment options that allow patients to ease their pain and regain control over their lives without medications or invasive procedures. Below, we’ll look at how Neurofunctional Pain Management may help ease cluster headaches in a drug-free, non-invasive way. Let’s get started.
What Is A Cluster Headache?
Cluster headaches are a type of trigeminal autonomic cephalgias (TACs), or a type of pain located in the head that derives from dysfunctions of the trigeminal nerve. This nerve is composed of a set of cranial nerve endings that stem from the side of the head – just above the ear – and spread to areas of the face such as your forehead, cheekbones, eyes, and jaw. The trigeminal nerve plays a vital role in delivering signals to the brain relating to muscle movements and sensations such as heat or pain.
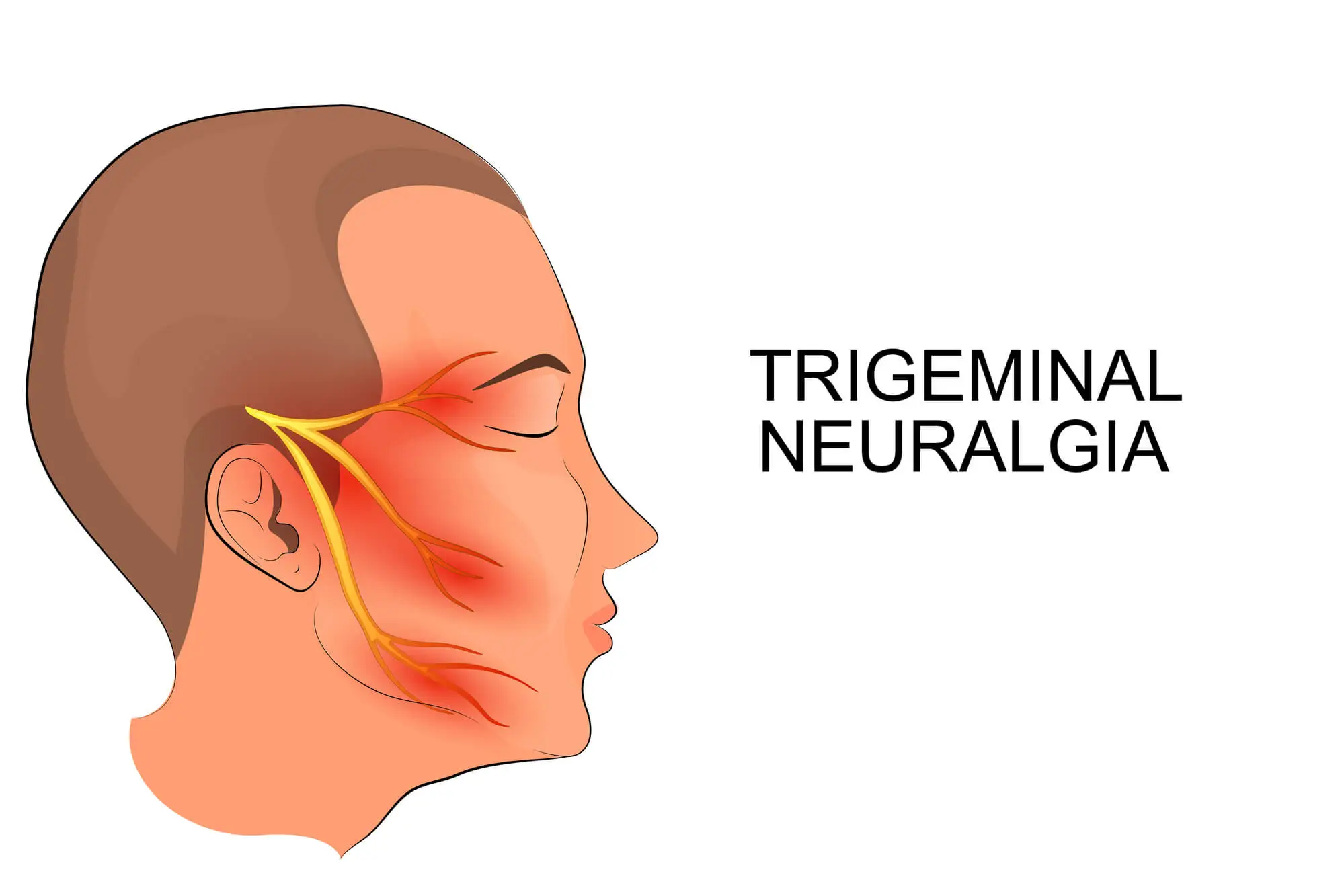
Although the reasons behind cluster headaches are not fully understood, the trigeminal nerve may play a role in most cluster headache attacks. When this nerve overreacts to stimuli and misfires, it leads to pain and other symptoms such as nasal congestion, lacrimation, and conjunctival injection.
While the symptoms of cluster headaches overlap those of other types of headaches, this condition has some unique features that help in the diagnostic process. Let’s look at these features:
- Frequency: During an attack, headaches occur 1-8 times a day. Each attack can last 2 weeks to 3 months and, between attacks, you may have remission periods during which you don’t experience headaches (these may last a minimum of 2 weeks).
- Short headaches: Cluster headache reaches full intensity quickly, usually within 5-10 minutes. Each headache usually lasts between 15 minutes and 3 hours before disappearing at the same speed it developed.
- Unilateral: Cluster headaches are often described as burning or stabbing pain that affects one side of the face. The side of the face affected may change from one attack to the next but rarely changes during the same attack. The pain is usually localized behind or around one eye and radiates through the forehead, nose, cheek, temple, and jaw. The painful sensations are accompanied by other symptoms, including tearing eyes, swelling, sweating, flushing, and tenderness in the scalp.
- Occurring at the same time: The hypothalamus, which is the component of the brain that homes our “internal biological clock”, may play a role in cluster headaches. Because of this, most patients with cluster headaches experience pain at the same time each day, most often at nighttime.
Although each headache is relatively brief, the pain can be intense, keep you awake at night, and be life-limiting. What’s more, most people affected by cluster headaches will experience cluster periods (bouts of frequent attacks) that last for months at a time before a remission period.
Cluster headaches may be chronic or episodic, depending on the frequency of the attacks and the length of the remission periods. Let’s look at these types of cluster headaches below.
Episodic Cluster Headache
As seen above, a cluster of headaches can last between 2 weeks and 3 months. During this period, you may experience headaches every other day or up to eight times a day. You have an episodic cluster headache if you have pain-free periods that last at least three months.
Many people with episodic cluster headaches have seasonal headaches. In this case, the cluster is triggered by the change of temperatures in spring or autumn, each time every year.
Chronic Cluster Headache
If you don’t experience any breaks between clusters, or the periods of remission are shorter than three months, your condition is categorized as “chronic”. Chronic cluster headaches affect 2 out of 10 people with cluster headaches and can be severely debilitating.
Associated Symptoms Of Cluster Headache
Cluster headaches are rarer – but more severe – than migraines, but many patients are affected by more than one type of head pain. Cluster headaches reach full intensity in just a few minutes and can lead to excruciating pain that often affects one side of the head.
Cluster headaches can affect your life for weeks or months at a time, and tend to recur at the same time each day. Nighttime headaches are often more severe than the ones you may experience during the daytime and lead to sleep disturbances and sleep deprivation.
This pain and lack of sleep can prevent you from being productive at work and lead to inhibited concentration and restlessness.
Below, we’ll look at the telltale signs that you may have cluster headaches.
- Tip: If your symptoms last for 2 days or more, and you are experiencing abnormal symptoms like shortness of breath, nosebleeds, vision loss, or high fever, you should seek emergency medical care immediately.
Pain on One Side of the Head and Around the Eye
Because cluster headaches involve the trigeminal nerve, the pain will be localized around one side of the face. The pain may move from one side of the face to the other in different attacks, but rarely within the same attack.
You are also likely to experience piercing and stabbing sensations accompanied by throbbing pain and pulsating veins, usually behind or around one eye. The pain reaches maximum intensity in as little as 5-10 minutes and can last up to 3 hours before decreasing suddenly.
Unlike migraines, which usually cause you to seek rest in a dark and silent room, cluster headaches may make you restless and agitated. It isn’t unlikely for people with cluster headaches to rock back and forth while holding their head during an attack.
Nasal Congestion
People with cluster headaches may also experience temporary nasal congestion, a condition known as sinusitis.
Although the relation between the two disorders isn’t clear, a 2013 study provides two possible explanations for this symptom:
- Although cluster headaches have no known cause, experiencing nasal congestion may be a telltale sign that the headache is triggered by sinusitis and not the other way around.
- During cluster headaches, the autonomic functions of the trigeminal nerve may be affected. This means that this nerve is no longer able to control bodily functions we don’t have control over which leads to symptoms such as excessive sweating and nasal congestion.
Facial Sweating or Flushing
One of the symptoms of cluster headaches is excessive sweating and flushing, usually localized to the forehead and cheeks. The pattern of facial sweating had been analyzed by studies in 1987 and 1988, which concluded this symptom is caused by the reduced ability of the trigeminal nerve to control autonomic functions, such as sweating and temperature control.
Droopy Eyelid and/or Pupil Constriction
Droopy eyelids and pupil constriction (a smaller pupil in the eye) are symptoms of common comorbidity of cluster headaches – Horner’s syndrome.
This condition is present in 10% of those with cluster headaches and, in most cases, the symptoms only last during the main headache attack. However, in severe cases of prolonged or chronic cluster headaches, damage to the pathways that connect the facial muscles to the brain may cause permanent Horner’s syndrome-like symptoms.
Nausea and Vomiting
Cluster headaches share some similarities with other types of headache syndromes, such as migraines. And, some of the most common migraine-like accompanying symptoms in people with cluster headaches are nausea and vomiting.
These symptoms, especially when accompanied by seizures, changes in vision and alertness, and drowsiness may indicate that your condition requires immediate medical care.
Sensitivity to Light or Sound
Chronic headaches can cause you to experience sensitivity to light and sound, especially during an attack. This symptom is due to temporary changes in how the brain processes visual and auditory stimuli, which can make listening to sounds and looking at lights more painful than it should be.
In most cases, cluster attacks and single headaches strike suddenly and without warning. However, according to a 2018 study, around 7% of patients experience warning visual and auditory signs such as abnormal sensations, which are known as “aura”.
Sensitivity To Light And Sound
Sensitivity to light and sound can be a strange, uncomfortable condition that often leaves sufferers feeling out of control. It can make it challenging to get through the day, as normal activities become hard to bear, whether it’s going shopping under...
Cognitive Impairment
Cognitive impairment describes any decline in cognitive abilities, such as memory, language, problem-solving, and attention. Such impairments can be a sign of more serious conditions, such as dementia or Alzheimer's disease, but they can also be the result of...
Tiredness, Nausea, and Weakness
If you are struggling with chronic tiredness, weakness, and nausea, you may be battling limitations in all aspects of your everyday life - from reduced productivity at work to pain, discomfort, and low energy levels. And the situation may be made worse by the...
Difficulty Focusing
Difficulty focusing or concentrating refers to the inability to maintain attention on a specific task for an extended period. It can manifest in various forms, such as being easily distracted, having trouble staying organized, and feeling overwhelmed by...
Dull Headache
Although many people will try to treat their dull headaches using over-the-counter (OTC) pain medications, doing so may not offer long-term relief. OTC medications only provide temporary relief from the symptoms and don’t treat the root cause. In addition,...
Fatigue And Irritability
Irritability and fatigue can significantly impact your quality of life by hindering daily activities and provoking distress. While treatment may be complicated, with an accurate diagnosis and early intervention, you can reduce the impact of tension headaches...
Throbbing Headache Only In Affected Areas
Throbbing pain is a common symptom associated with a range of headache types. It manifests itself as a rhythmic pulsing, beating, or pounding sensation that may affect just a part of the head or the whole head. Throbbing headaches are commonly caused by...
Pupil Constriction
A cluster headache is a type of headache that is characterized by severe, excruciating pain on one side of the head. It is often described as a stabbing or burning sensation lasting from 15 minutes to several hours. Cluster headaches typically occur in...
Causes Of Cluster Headache
Cluster headaches are considered primary headaches, which means that the pain is the condition, and no underlying problems are causing the pain. This is in contrast with secondary headaches, which can be caused by health conditions and events such as tumors, arterial tears, blood clots, and sinusitis.
This characteristic of cluster headaches, coupled with the fact that they are a rare condition, makes studying their causes and risk factors difficult at best. Because of this, in most cases, it isn’t clear what causes a cluster headache.
Nonetheless, you are likely to get a cluster headache when an external stimulus triggers one or more nerve pathways linked to the hypothalamus in the brain. The hypothalamus is responsible for managing several bodily functions such as sleep cycle, blood pressure, heart rate, body temperature, and sensations such as thirst.
Below, we’ll look at some common triggers of cluster headaches. However, it is important to notice that these triggers are not the root cause of cluster headaches, but rather the stimuli that may bring on an attack in patients already suffering from cluster headaches.
Understanding what triggers a new round of headaches can help you postpone or prevent an attack while extending the period of remission.
Let’s look at these risk factors and triggers below.
Genetic Factors
Males are 2.5 times more likely than women to suffer from cluster headaches. This condition can emerge at any age, but it is often diagnosed in adults aged 30 to 40. Additionally, individuals with a family member who has been diagnosed with cluster headaches are 5-18 times more at risk of developing this condition.
Substance Use
When you are in a cluster period, even a single alcoholic drink can trigger the attack.
Substance use can be the main factor that starts a cluster of headaches, but it can also increase your risk of developing this condition in your lifetime. Indeed, smokers are more likely to have cluster headaches.
Some substances that are risk factors for cluster headaches include:
- Tobacco and nicotine
- Alcohol
- Cocaine
Diet and Lifestyle
Some lifestyle factors may act as triggers for cluster headaches. These factors often create physical or psychological stress, which has an impact on the hypothalamus, the trigeminal nerve, and the nervous system as a whole. In turn, such high levels of stress make dysfunctions more likely.
These factors include:
- Sleep deprivation
- Exertion
- Eating foods that contain nitrates, such as bacon.
Environmental Triggers
Environmental changes are among the greatest risk factors for cluster headache attacks. Firstly, most patients’ attacks are related to changes in seasons. Allergies and other conditions such as sinusitis, coupled with rapid temperature changes, can trigger a cluster of headaches. Some people with this condition often mistake cluster headaches for allergies or stress.
Some other environmental factors that might cause an attack when you are in a cluster period include:
- Extreme cold or extreme heat
- Sudden temperature changes
- Sudden changes in altitude
- Strong smells and bright lights
Stress and Anxiety
High levels of stress, as well as emotional and psychological disorders such as anxiety, are recognized risk factors for migraines and other types of headaches. Studies conducted in 2006 have now linked extreme emotional stress to cluster headache attacks as well.
Cluster Headache Diagnosis
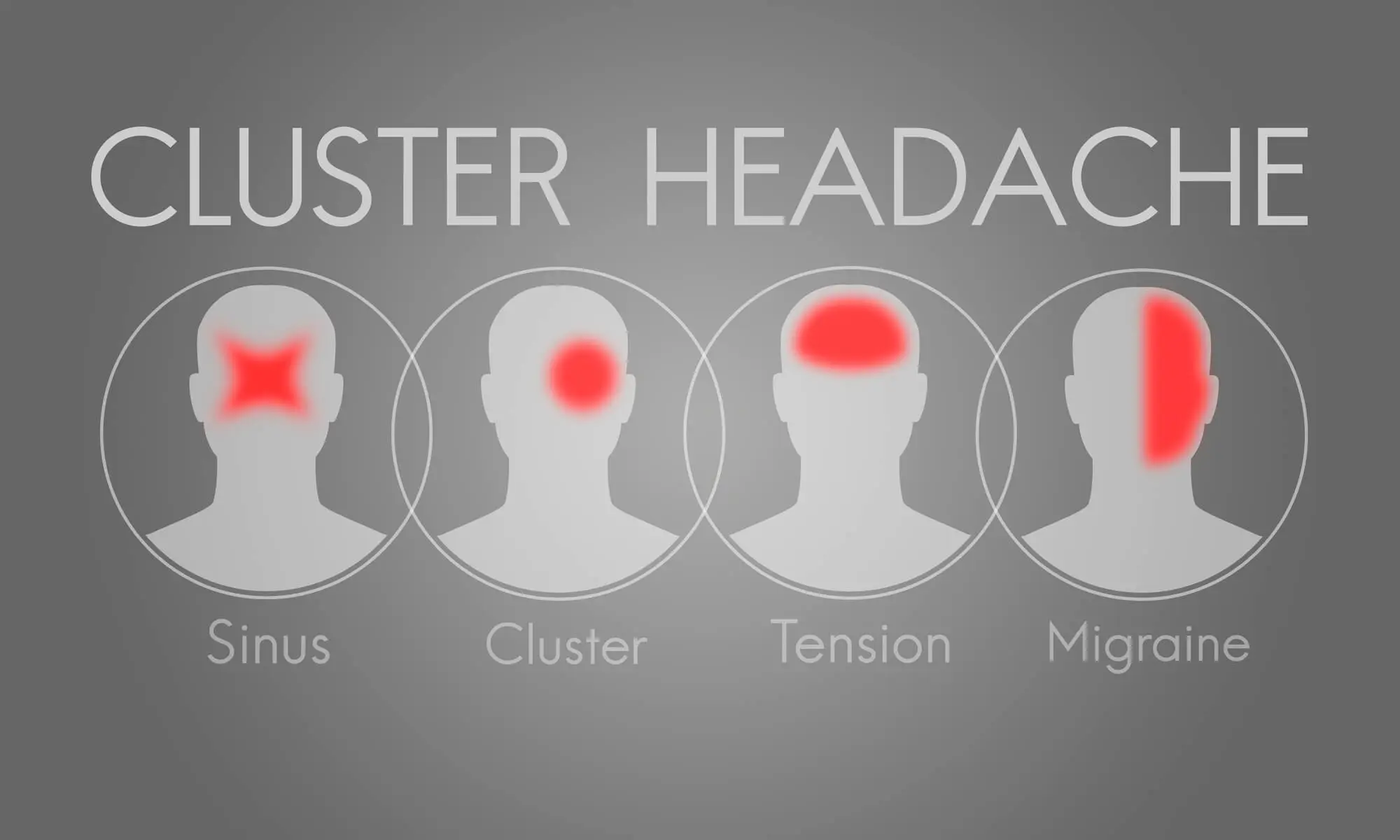
Because of how rare cluster headaches are, they are often misdiagnosed for other types of headache syndromes, as well as sinusitis and seasonal allergies.
Additionally, there is no test specifically designed to diagnose cluster headaches. A specialist will usually combine a range of exams and tests to determine what type of headache syndrome you have, or whether the pain derives from an underlying health condition.
Some of these assessments include:
- An evaluation of your medical history
- An evaluation of risk factors (i.e.: being between 20 and 40 years old, being male, being a smoker, etc.).
- A review of the nature and pattern of your symptoms, such as the location of the pain and the frequency of attacks
- Neurological examinations
- Brain scans and imaging tests (often used to rule out underlying brain conditions)
Patients with cluster headaches often receive a diagnosis from a neurologist or other headache specialist.
Common Headache Misdiagnosis
As seen above, the symptoms of cluster headaches overlap with the ones of other conditions. This, coupled with the fact that over 200 types of headaches have already been identified, makes it harder for patients to receive a timely and accurate diagnosis.
Generally, cluster headaches are primary headaches. This means that they are not caused by an underlying illness, and the pain is, in itself, the condition. However, cluster headaches are often misdiagnosed for other secondary health conditions that could be causing pain to the head, such as:
- Seasonal allergies and allergic reactions
- Head trauma and injuries
- Exertion due to intense physical activity
- Caffeine overuse or withdrawal
- Hormone imbalances and fluctuations, such as the ones occurring during pregnancy or menstrual cycles
- Hormonal changes caused by birth control pills
- Medication use
- High blood pressure
- Stress
According to a study conducted in 2000, people with cluster headaches experience a delay of nearly 7 years before obtaining a diagnosis and have to consult an average of 4.3 physicians to be correctly diagnosed.
And, being misdiagnosed isn’t inconsequential. Firstly, over 70% of those with cluster headaches end up undergoing unnecessary magnetic resonance and other scans, while 4% of them face unnecessary surgical procedures to correct their sinus or a deviated septum.
Ultimately, obtaining the right diagnosis is the first step to finding an adequate treatment for cluster headaches. Let’s look at the treatment options available in more detail below.
Medical Treatment Options For Cluster Headache
Although cluster headaches are considered rare, for people who suffer from this condition, their pain can be excruciating and life-limiting. To understand to what extent cluster headaches affect a person’s life, it is enough to say that this type of headache is sometimes referred to as a “suicide headache”. This is due to the increased suicidality of patients who are experiencing or anticipating a cluster headache.
While there is no permanent cure for cluster headaches, your physician is likely to recommend two lines of treatment:
- Acute treatment: Acute attack treatments are emergency medications taken to help while a cluster attack is underway. They aim to stop or alleviate the pain.
- Preventive treatment: Preventive measures aim to decrease the intensity and frequency of attacks, and they are usually administered during the remission period. These treatments involve medications as well as lifestyle and dietary changes.
Let’s look at the most common lines of treatments recommended by physicians for cluster headaches.
Medication
Several medications are prescribed to ease the intensity of a cluster attack and prevent more attacks from happening. These are delivered as nasal sprays, injections, or capsules, and include:
- Pain relievers (i.e.: triptans, such as sumatriptan and zolmitriptan, and lidocaine)
- Lab-made growth hormones (i.e.: octreotide)
- Supplements (i.e.: melatonin and capsaicin)
Preventive medications that may be able to stop attacks before they happen include corticosteroids like prednisone, lithium carbonate, verapamil, and divalproex sodium.

One of the most efficient treatments for attacks that are already underway is inhaling pure oxygen. This treatment is delivered by a specialized professional through a face mask, usually in intervals of 15 minutes.
If your condition does not respond to these treatments, you may resort to other options, such as occipital nerve blocks. An occipital nerve injection will deliver steroids and anesthetic into the nerves at the base of the skull, which are often the starting point for cluster headaches.
While these lines of treatment may be helpful in the short term, it is important to notice that pain relievers, non-steroidal anti-inflammatory drugs (NSAIDs), and corticosteroid injections come with severe side effects, including addiction.
What’s more, the same 2000 study cited above highlights the fact that many patients with cluster headaches, because of their misdiagnosis, are prescribed inappropriate medications such as antibiotics and propranolol. These are not only ineffective, but can also cause side effects such as nausea, diarrhea, and vomiting.
Exercise
Exercise can benefit people with cluster headaches both directly and indirectly.
Firstly, daily physical activity may boost sleep quality, reduce stress, and trigger the release of the body’s natural painkillers, endorphins. Additionally, living an active lifestyle, while reducing the consumption of alcohol and nicotine may improve blood circulation and keep at bay health conditions such as headache disorders.
If you suffer from cluster headaches, moderate exercise can help prevent and alleviate attacks. In particular, you may benefit from practicing mind-body disciplines like yoga and breathing exercises. Let’s look at the benefits of these activities below:
- Breathing exercises: As seen above, inhaling 100% oxygen for around 15 minutes may reduce the intensity of cluster headaches. If you don’t have pure oxygen at hand you can’t access immediate medical care, breathing exercises may help. Techniques such as deep breathing, visualized breathing, and rhythmic breathing can increase the levels of oxygen in the blood and relieve stress.
- Yoga and tai-chi: Disciplines like yoga and tai-chi may help you manage stress levels, which can reduce the likelihood of cluster attacks. What’s more, gentle stretches can reduce muscle tension, which can aggravate ongoing headaches.
Massage and Physical Therapy
Complementary therapies such as massages and physical therapy can have a pain-relieving effect on cluster headaches. Indeed, massages have been seen to trigger the release of pain-killing, feel-good hormones such as endorphins. Additionally, massages and physical therapy can improve the body’s conditioning, boost blood and oxygen circulation, reduce muscle tension, and lower stress levels.
Some self-massage techniques that may help include pressing with the thumbs just about the bridge of the nose, performing circular movements on the temples, and lightly pinching your eyebrows, all while taking deep breaths.
This line of treatment isn’t equally effective for everyone, and it is contraindicated for people with head trauma or injuries. Make sure to consult a therapist to avoid aggravating your condition.
How Neurofunctional Pain Management Manages Cluster Headaches
Fortunately, taking medications daily, resorting to occipital nerve injections, or undergoing surgery are no longer the only options available to patients to manage their condition.
Thanks to Neurofunctional Pain Management programs, patients may be able to reduce their pain and improve their quality of life without medications or invasive procedures. Here’s what to expect from Neurofunctional Pain Management:
Electroanalgesia
Electroanalgesia is a pain management technique that uses high-pulse electrical current to ease pain, boost blood circulation, improve mobility, and induce...
IV Therapy
IV nutritional therapy, or intravenous therapy, involves administering vital nutrients directly to the bloodstream through an IV. This type of treatment bypasses the digestive system, allowing for maximum absorption and utilization of nutrients by the...
Lifestyle Counseling
Lifestyle counseling is an approach to managing chronic pain that involves identifying, assessing, and modifying lifestyle factors contributing to an individual's pain. For example, lifestyle factors such as nutrition, physical activity, stress, sleep quality...
Start Managing Cluster Headache Pain
If you are tired of taking medications for months at a time or live in fear of having to undergo surgery to ease the pain from your headaches, you are certainly not alone. However, thanks to the Neuragenex Neurofunctional Pain Management approach, you may now find a solution to your pain without drugs or surgery.
Get proper pain management for cluster headaches.



