Endometriosis

Addressing Endometriosis Pain With Intercourse
Read More
June 29, 2023
Over 6.5 million people in the US alone see their lives entirely disrupted by endometriosis – a condition that causes the abnormal growth of the lining of the uterus (endometrial implants) on other organs, including the ovaries, fallopian tubes, bladder, and pelvic cavity.
Endometriosis isn’t always painful, but leaving it unaddressed inevitably leads to life-limiting consequences, regardless of whether you experience symptoms or not.
For example, if you experience pain during periods or sex, these symptoms can cause distress and get in the way of your personal, professional, and intimate life. On the other hand, if you only have mild discomfort that can be mistaken for normal menstrual cramps, the endometrial implants can continue growing undetected on other organs, leading to infertility.
Learning to identify the early signs of endometriosis can help you address the risk factors of this condition, avoid its most severe complications, and find the best treatment option for you. Get started with the guide below.
In people with endometriosis, the lining of the uterus (endometrium) grows outside of the uterus, on nearby tissues and organs. In healthy reproductive systems, the endometrium plays a vital role during the early stages of pregnancy by supporting the growth of the fetus and protecting it from harmful microbes.
The endometrium thickens during the follicular phase of the menstrual cycle in preparation for a mature egg. If the egg isn’t fertilized and a pregnancy does not occur, the endometrium inside the uterus is then expelled during the menstruation (period). New endometrium is created with each menstrual cycle.
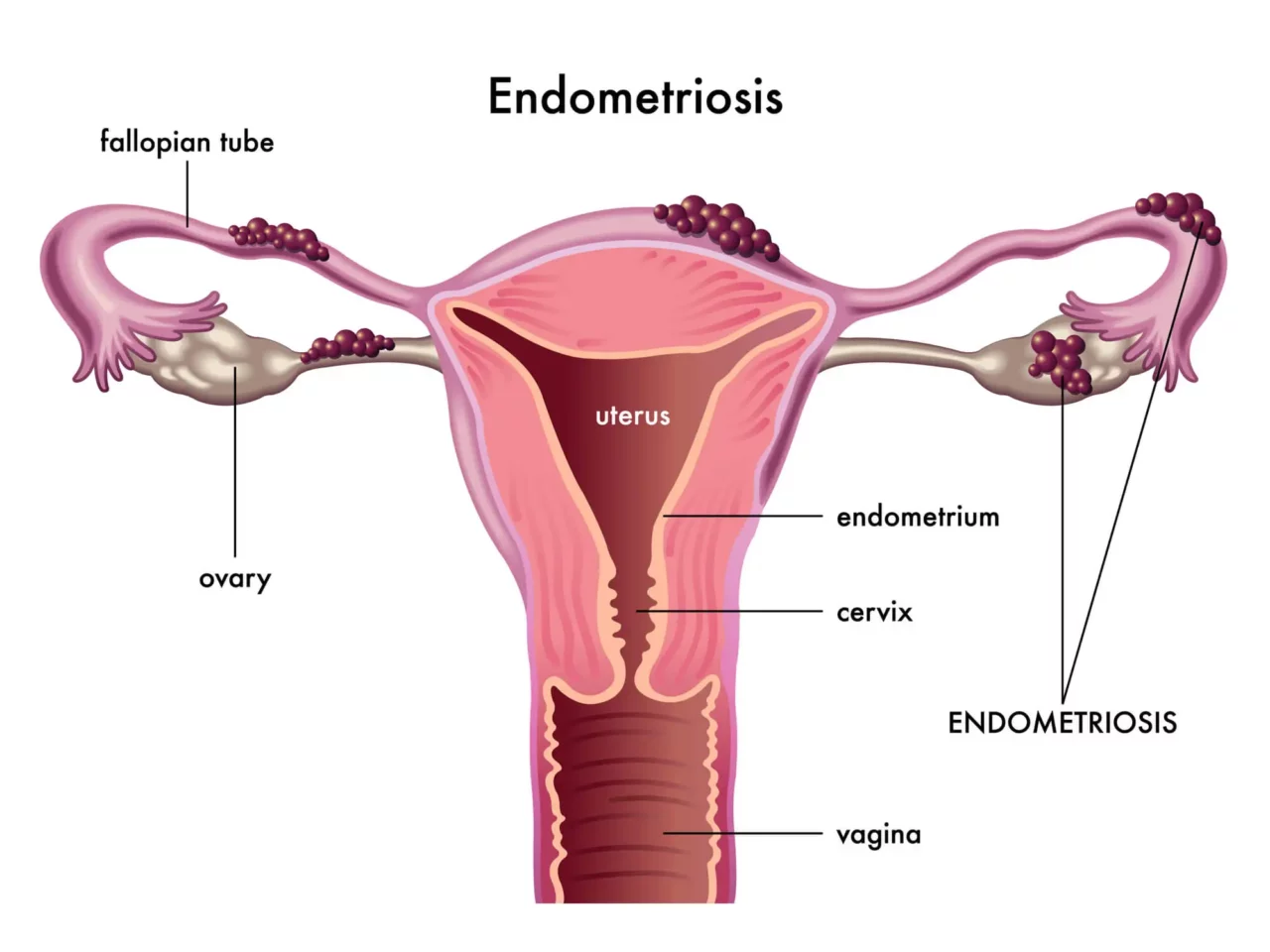
Endometriosis occurs when the endometrium begins to grow outside of the uterus. This abnormal endometrial tissue, which is known as endometrial implants, can grow on surrounding areas such as the ovaries, bladder, pelvic cavity, rectum, cervix, and exterior walls of the uterus.
The endometrial implants grow and swell during each menstrual cycle, behaving similarly to the endometrium inside the uterus. However, unlike normal endometrium, endometrial implants are unable to leave the body during your period.
Over time, the build-up of abnormal endometrial implants leads to a cascade of complications, including:
As the endometrial implants begin to build up outside of the uterus, you may notice a range of symptoms. Learning to identify them can help you prevent dangerous cysts and lifelong problems like infertility.
It is estimated that 80% of women with dysmenorrhea have endometriosis, making painful periods one of the most common symptoms of this condition.
However, painful menstruation may seem like a normal aspect of a woman’s menstrual cycle, which causes many women with dysmenorrhea to simply dismiss this symptom. Although mild cramping and discomfort are normally associated with menstruation, it is important to clarify that dysmenorrhea is a severe condition that can worsen over time.
If you are unsure whether your painful periods are, in fact, a sign that you have endometriosis, look for other associated symptoms such as excessively painful cramps, back and abdominal pain that lasts long before and after your period, and heavy or prolonged bleeding.
If you have endometriosis, the pain you experience isn’t always correlated to the extent and location of the endometrial implants. So, you may have a mild form of endometriosis and experience excruciating pelvic pain. On the other hand, you may only experience mild discomfort even if the endometrial implants are widespread.
Regardless of how intense your pain is, if you have chronic (lasting longer than six months) or cyclic pain below your belly button, you should immediately undergo diagnostic tests for endometriosis. According to studies, up to 38% of people with chronic pelvic pain have endometriosis.
Pain during intercourse, or dyspareunia, is a symptom that affects over half of people with endometriosis. It can occur due to deep vaginal penetration because the thrusting that occurs during sexual intercourse further inflames and irritates the endometrial growth outside of the uterus.
Pain during intercourse can change depending on the phase of your menstrual cycle and can be mild or severe. It is often described as stabbing or sharp sensations that last long after having sex.
Deep dyspareunia is one of the reasons why over 66% of women with endometriosis also suffer from sexual dysfunction.
Endometriosis is sometimes associated with fatigue and personality changes. These symptoms are more noticeable during menstruation when the body attempts to eliminate the abnormal endometrial growths outside of the uterus and any diseased tissue. During this phase of the menstrual cycle, the body’s immune system also triggers the release of inflammatory toxins known as cytokines, in an effort to fight endometriosis.
As a result of these chemical processes, you’ll feel constantly fatigued and physically exhausted, especially during menstruation. Although this symptom is sometimes dismissed by healthcare providers, it is crucial to undergo the necessary diagnostic tests before severe symptoms of endometriosis appear.
Although mild bloating may be a common denominator of several health conditions, up to 96% of women with endometriosis will experience several gastrointestinal problems known as “endo belly”. These digestive issues include constipation, diarrhea, bloating, and nausea.
“Endo belly” arises from a range of processes and reactions. Firstly, people with endometriosis may have gastrointestinal bacterial overgrowth, which can impact the normal functioning of the digestive processes. Additionally, the high levels of inflammation caused by the growing endometrial implants can irritate the surrounding tissues and cause water retention, which can cause your pelvic area to appear bloated.
If you suffer from endometriosis, over time, the abnormal endometrial implants may begin to spread to surrounding organs, including the bowel, rectum, and intestines. When this happens, the endometrial implants can cause sustained inflammation, irritation, and lesions to the surrounding tissues.
Over time, this can impact the normal functioning of your bowel and digestive organs, leading to painful and irregular bowel movements, especially when the endometrium is swelling or thickening (i.e.: during the luteal phase). It is also estimated that up to 52% of women with endometriosis also have irritable bowel syndrome (IBS).
Endometriosis can affect the health and function of the bladder in two different ways.
Firstly, ovarian cysts caused by trapped blood in the ovaries can lead to urinary problems by pressure on the bladder. Additionally, if the endometrial implants begin to grow on the bladder and surrounding organs, you may experience several symptoms, such as:
These symptoms tend to intensify in the days before your period and during your menstruation.
Infertility and endometriosis are often connected. Research published in the Journal of Assisted Reproduction and Genetics reports that up to 50% of infertile women have endometriosis and that half of those with endometriosis are infertile.
Infertility in people with endometriosis is often caused by endometrial implants that cause adhesions between organs and scar tissue. The abnormal growth of endometrial tissue can block the fallopian tubes and prevent the release of mature eggs into the uterus, preventing pregnancy. Excessive endometrial growth can also inhibit the action of the sperm or damage a fertilized egg before its implantation in the uterus.
It is also important to notice that endometriosis can cause sexual dysfunction in otherwise fertile women, which makes it more difficult to conceive.
Although some women with endometriosis are infertile, others only experience temporary infertility and are able to carry a baby to term successfully following adequate treatment. Other alternatives, such as in-vitro fertilization (IVF) can assist patients with endometriosis looking to have a baby.
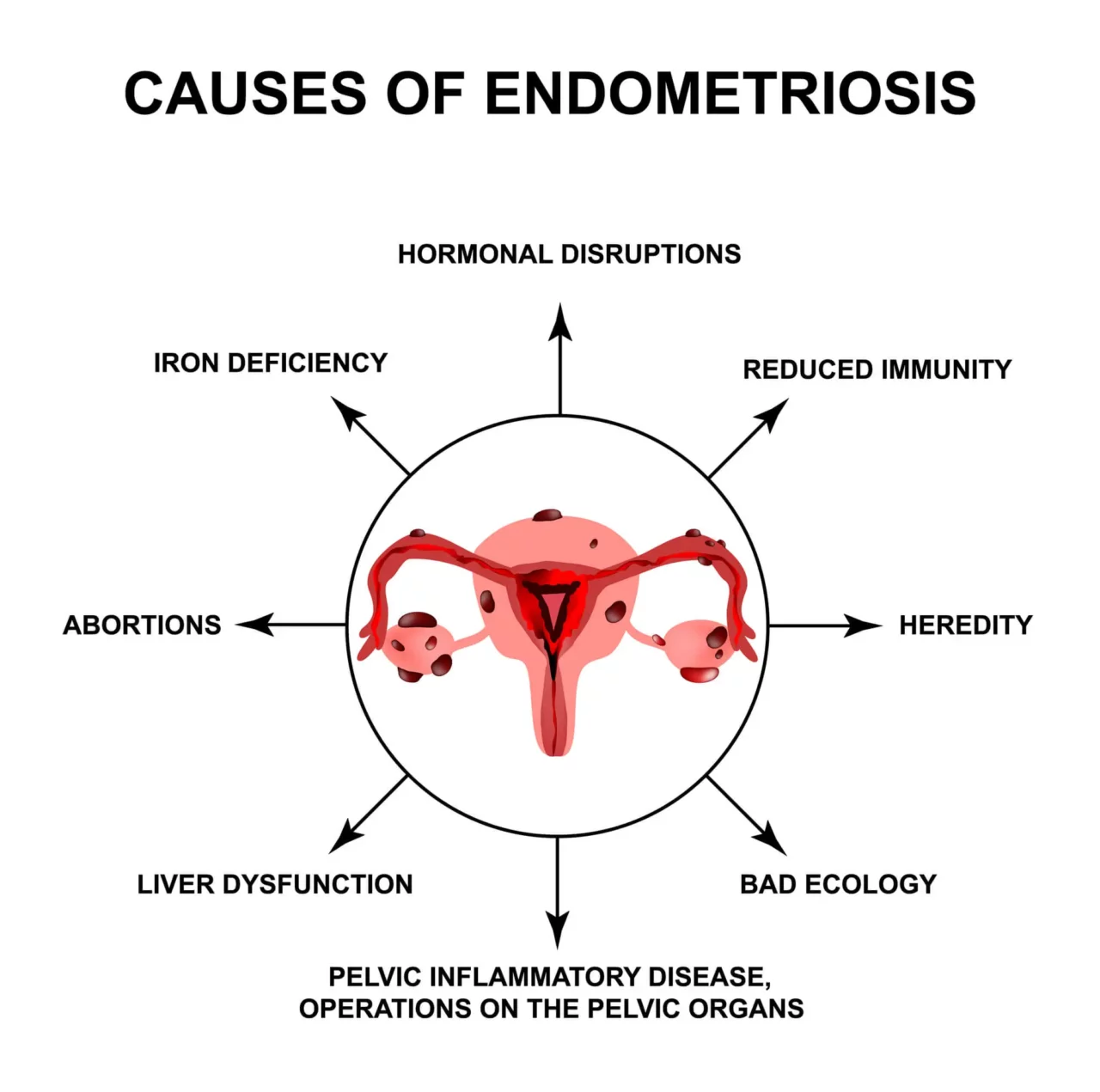
The causes and risk factors of endometriosis aren’t always clear. According to different theories, endometriosis occurs when the endometrial tissue in the uterus is spread to nearby organs and tissues. This can happen due to surgery such as a C-section or retrograde menstruation, which occurs when part of the menstrual blood carrying endometrial tissue flows back into fallopian tubes instead of leaving the body during menstruation.
Besides these causes, several risk factors can make you more prone to developing endometriosis. Being aware of these risk factors can help you undergo the necessary screening tests early on and address the condition as the first symptoms occur.
Let’s start by looking at the factors that put you at risk of endometriosis.
Endometriosis may occur at any point after the onset of the menstrual cycle (menarche). The symptoms of endometriosis may decline during pregnancy and disappear after menopause.
Unfortunately, the majority of women with endometriosis are only able to obtain an accurate diagnosis when they are trying to conceive, or if they are looking into the causes of unexplained infertility. However, this delay in getting a diagnosis – which can be as long as seven years – isn’t necessarily related to the lack of symptoms.
According to estimations, only around 20% of cases of endometriosis are asymptomatic, while 80% of women with this condition experience painful periods, excessive bleeding, digestive issues, and pain during intercourse. At the same time, the majority of women with endometriosis are disbelieved or dismissed by their healthcare providers, which can prevent them from obtaining an adequate diagnosis.
Fortunately, the increased understanding of the symptoms and prognosis of endometriosis has encouraged developments in the diagnostic tools used and highlighted the importance of early awareness.
Some of the strategies used to diagnose endometriosis today include:
Advocating for your own health and working with a specialist who can help you obtain an accurate diagnosis for your pelvic pain can help you prevent severe complications, like cysts, scars, and infertility.
Endometriosis is considered to be a lifelong condition for which there is no definitive cure. However, your healthcare provider may recommend the following treatment approaches to manage your symptoms:
Before choosing a certain line of treatment, it is important to determine what your goals are. For example, if you are hoping to conceive, birth control pills and irreversible surgical procedures such as hysterectomy are not suitable choices. What’s more, in around 20% of cases, surgical procedures for endometriosis are inefficient, leaving patients to seek an alternative treatment option.
If you suffer from endometriosis, you may be battling the prospect of living a life reliant on medications or undergoing invasive surgical procedures. Fortunately, non-surgical, non-invasive, and non-pharmaceutical treatment options that are efficient in easing the symptoms of endometriosis and slowing down the progression of this disease exist.
The whole-person Neurofunctional Pain Management approach pioneered by Relatyv combines several therapies to help you regain your pelvic health and lay the foundations of long-term health. These include:
About the Author
Will is a healthcare executive, innovator, entrepreneur, inventor, and writer with a wide range of experience in the medical field. Will has multiple degrees in a wide range of subjects that give depth to his capability as an entrepreneur and capacity to operate as an innovative healthcare executive.
Share on Social Media


You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/
You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/
Neurofunctional Pain Management Overview
Symptoms
Conditions Treated
Treatments
Articles by Category
Locations
Colorado
Wisconsin
Georgia
Hiram
Lawrenceville
Marietta
Powder Springs
Texas
Waco
Victoria
Illinois
Buffalo Grove
New Lenox
St. Charles
Arizona
Tucson
Waddell
Arlington
Avondale
Buckeye
Superior
Mesa
Palo Verde
Morristown
Tempe
Chandler
Anthem
Eloy
Florence
Fort McDowell
Phoenix
El Mirage
Coolidge
Gilbert
Arizona City
Casa Grande
Casa Blanca
Aguila
Sacaton
Apache Junction
Kearny
Stanfield
Goodyear
Litchfield Park
Alabama
Arkansas
California
Florida
Idaho
Indiana
Iowa
Kansas
Louisiana
Maryland
Michigan
Rhode Island
Minnesota
Mississippi
Nevada
New Jersey
New Mexico
North Carolina
Ohio
Pennsylvania
South Dakota
Tennessee
Utah
Virginia
Washington

