Abstract
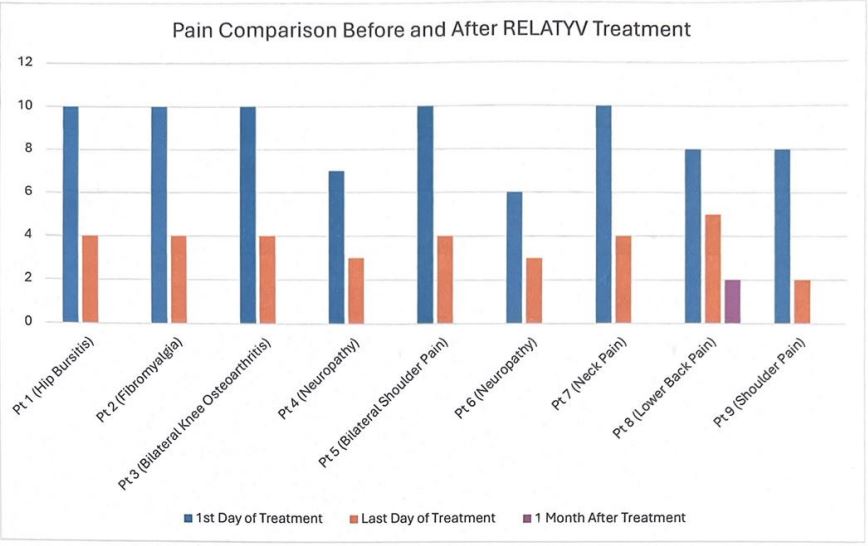
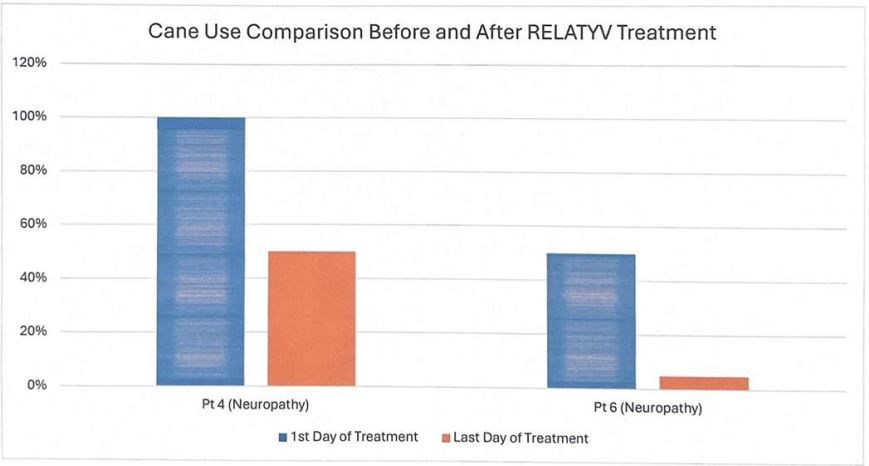
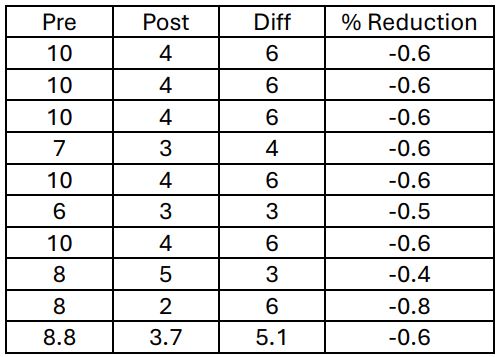
Neurofunctional Pain Management, NFPM, a non-pharmaceutical, non-surgical, noninvasive, and non-chiropractic therapy protocol comprising a combination therapy of high pulse electroanalgesia, IV nutritional hydration, and health coaching has shown to be an effective method of reducing chronic pain and improving balance in participants who completed a normal course of therapy. In this study, nine participants experienced a significant reduction in chronic pain representing an average pain score drop from 8.8 to 3.7 on a standard 0-10 pain scale. This reflects a 60% reduction in pain on average. Two participants using canes for mobilization recorded reduced utilization in cane use, reflecting an improved balance in addition to a reduction in pain. One participant documented a 50% reduction in cane use, while the other documented a 90% reduction in cane use. This study shows that NFPM may be an effective treatment option for patients suffering from a variety of chronic pain conditions as well as improve the safety and mobility of patients using canes or walkers.
Introduction
Chronic pain is a pervasive and ongoing medical problem that creates many difficulties for both patients and providers. Traditional pharmaceutical therapies are often ineffective, may reduce in efficacy over time, and frequently create undesirable side effects and medication interactions. Non-pharmaceutical, non-surgical, and non-invasive treatment options for chronic rare and often do not provide relief sufficient to significantly impact the patient’s quality of life.
Most pain management providers would define pain relief success with a chronic pain condition to be anything greater than a 30% reduction in pain. According to a study published in The Journal of Pain, a 30% or greater reduction in pain resulted in a pain relief outcome that the patient felt was significantly valid in improving their quality of life. “Changes of approximately 2.0 points or 30% to 36% represent “much better,” “much improved,” or “meaningful” decreases in chronic pain, and a decrease of ≥4 points or ≥50% appears to represent a substantial (“very much improved”) change in pain, 1 which patients have also considered “treatment success”112 or “satisfactory improvement.” (Dworkin et al., 2009)
Neurofunctional Pain Management, NFPM, presents as an impressive alternative to pharmaceutical and conventional pain treatment options. NFPM is a combination of high frequency high-pulse electroanalgesia electrical currents which penetrate deep tissues to create neural tissue modulation and sustained depolarization, specialized vitamin/mineral IV hydration, and targeted health coaching to produce effective and lasting pain relief for patients suffering from chronic pain.
This combination of therapies that comprise the NFPM protocol produces a substantial pain relief effect as demonstrated by this study data, resulting in a near 60% resolution of chronic pain and a 90% reduction in cane use as reported by one of the participants. This level of pain relief derived through non-pharmaceutical options offers medical providers an excellent opportunity to help their patients who suffer from debilitating chronic pain and resulting imbalance and reduced mobility, particularly when pharmaceutical options have proven ineffective, and dosing of various medications poses too great a risk to the patient.
Methods
This study consists of secondary data collected from medical practices groups conducting an eight-week Neurofunctional Pain Management treatment protocol. Patients in this treatment protocol were screened by a qualified medical provider and were issued orders for a treatment program that consisted of two treatment events per week. Each eventconsisted of a 53 min treatment cycle of electroanalgesia therapy with one of these events including a concurrent one-liter vitamin/mineral blend IV infusion. The patient also received a 30min session of health coaching with each treatment event. This combination of activities resulted in the pain relief outcomes demonstrated by the results data shown below.
Results
The full study consisted of 9 participants with chronic pain and two of those participants with regular documented cane use for mobility, stability, and balance. After completing an 8-week course of treatment with NFPM the average pain reduction point drop was 5.1 on a 0-10 pain scale, which reflects a 60% reduction in pain on average. A pain reduction outcome that, by the standards established via Dworkin et al, above would be considered a tremendous success for chronic pain reduction. The average starting pain score was 8.8 and reduced to 3.7 over an eight-week treatment regimen which consisted of two treatment events per week. This reflects an average 60% pain reduction for the population of the study.
Discussion
This study data concludes that Neurofunctional Pain Management, a non-pharmaceutical, non- surgical, non-invasive, and non-chiropractic treatment modality, is capable of producing a significant reduction in chronic pain across a variety of chronic pain conditions, as indicated by the results above. This further demonstrates that NFPM may
prove effective as a first option therapy before the use of medications, surgery, or invasive procedures, and could be a significant contribution to the treatment of chronic pain at the primary care level. The results further support the national and worldwide effort to avoid dangerous and addictive narcotic medications in the treatment of chronic pain.
Pain score data is collected at each treatment event, making it convenient to identify. A wide range of health improvements and quality of life improvements reported by participants as a result of the NFPM treatment program are improved sleep, reduced stress, improved breathing and even reduced blood pressure. None of these topics were included in this study as data points at this time but may be utilized in further studies.
Further research is needed to determine if NFPM should be considered a first option standard course of care at the primary care level before a patient is referred to or considered for interventional procedures or surgeries. Further research is needed to determine if NFPM should be considered a first option before prescribing narcotic, opioid, or addictive pharmaceutical options. With the efficacy rate shown in this study, and knowing that NFPM is a non-invasive therapy, it is possible that NFPM could be integrated into the medical decision-making process as a required prior therapy option.
Conclusion
Neurofunctional Pain Management has shown to be a viable treatment option for patients suffering from chronic pain, showing a 60% pain reduction result for the participant in this study. NFPM may be able to replace many current conventional therapies for chronic pain. NFPM may offer patients and medical providers with a better first choice treatment option that is non-pharmaceutical, non-surgical, non-chiropractic, and non-invasive.
References
1) Bozeman, W. (2023, July 6). Electroanalgesia treatment within neurofunctional pain management. Neuragenex. https://neuragenex.com/modality/electroanalgesia/
2) Dworkin, R. H., Turk, D. C., McDermott, M. P., Peirce-Sandner, S., Burke, L. B., Cowan, P., Farrar, J. T., Hertz, S., Raja, S. N., Rappaport, B. A., Rauschkolb, C., & Sampaio, C. (2009). Interpreting the clinical importance of group differences in Chronic pain clinical trials: Immpact recommendations. Pain, 146(3), 238–244. https://doi.org/10.1016/j.pain.2009.08.019
3) Limoge, A., & Stanley, T. (2006). Electroanalgesia, systemic. Encyclopedia of Medical Devices and Instrumentation. https://doi.org/10.1002/0471732877.emd089
4) Robb, K. A., Newham, D. J., & Williams, J. E. (2007). Transcutaneous electrical nerve stimulation vs. transcutaneous spinal electroanalgesia for chronic pain associated with breast cancer treatments. Journal of Pain and Symptom Management, 33(4), 410–419. https://doi.org/10.1016/j.jpainsymman.2006.09.020
5) Schwartz, R. G. (1998). Electric sympathetic block: Current theoretical concepts and clinical results. Journal of Back and Musculoskeletal Rehabilitation, 10(1), 31– 46. https://doi.org/10.3233/bmr-1998-10105
6) Wang, S.-M. (2016). Electroanalgesia in pain management. Integrative Pain Management, 469–482. https://doi.org/10.1093/med/9780199315246.003.0033
7) White, P. F., Elvir Lazo, O. L., Galeas, L., & Cao, X. (2017). Use of Electroanalgesia and Laser Therapies as alternatives to opioids for acute and chronic pain management. F1000Research, 6, 2161. https://doi.org/10.12688/f1000research.12324.1
8) White, P. F., Li, S., & Chiu, J. W. (2001). Electroanalgesia: Its role in acute and chronic pain management. Anesthesia & Analgesia, 92(2), 505–513.
https://doi.org/10.1213/00000539-200102000-00042